Rewinding back to the beginning of the case, hours before the above CXR...
A middle-aged man with no PMH p/w progressive shortness of breath x several months. He normally has a “smoker’s cough” but recently his cough has increased and he is finding it harder to breathe.
T 98, HR 98, BP 110/70, RR 20, SpO2 92% on 2L. Exam revealed reduced breath sounds R chest, dullness to percussion of R chest, reduced R sided tactile fremitus. CXR revealed opacification of R hemithorax with slight left mediastinal shift. Seemed c/w pleural effusion.
R lung, upper anterior chest
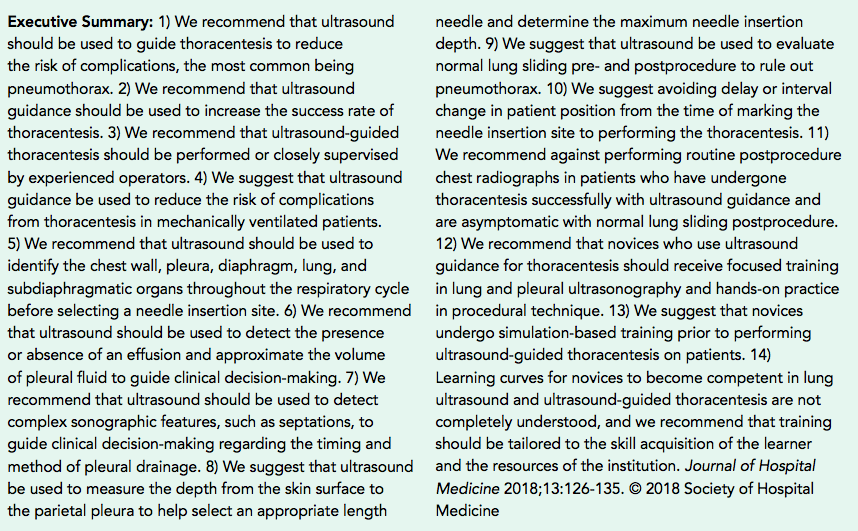
1) Should US always be used for thora?
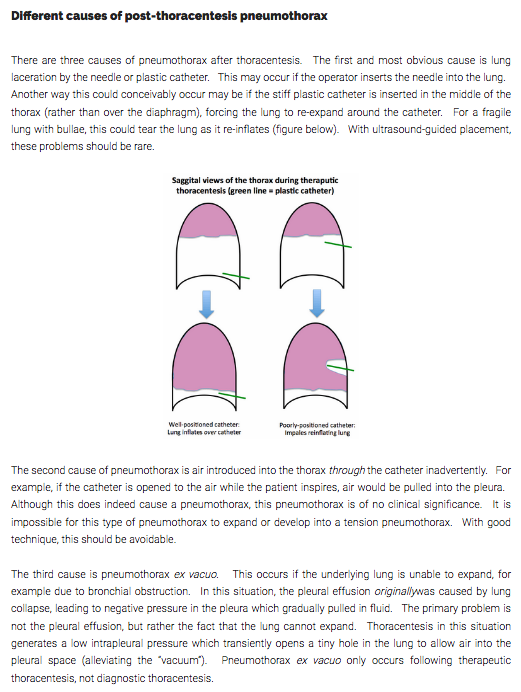
2) Causes of post-thoracentesis PTX
3) Physiology of PTX ex vacuo? how to recognize and manage?
4) Should we routinely measure pleural pressures during thora?
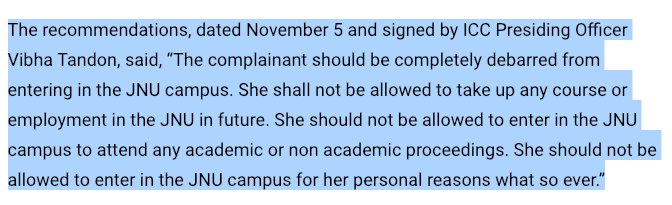
14/
15/
-lung laceration by needle or catheter
-bleb rupture
-unintentional air entry through catheter (can ppx w 1 way tubing. stopcock can help but not perfect)
-non-reexpandable lung (PTX ex vacuo)
emcrit.org/pulmcrit/pneum…
17/
-trapped lung (thick visceral pleural rind). Maye amenable to decortication
or
-lung entrapment (collapsed portion of lung, often due to malignancy). Not for decortication (note effusion often transudative, due to pressure mechanism)
19/
21/
Data seems equivocal. Might consider if concern for trapped lung. Thanks to @BegMoeez for reference thelancet.com/journals/lanre…
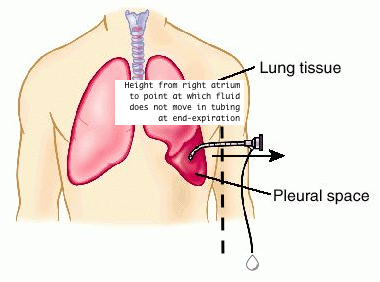
Does anyone do this w/ simple tubing (as below), rather than dedicated manometer? Or too imprecise?
22/
-POCUS is key in performing thoracentesis
-PTX ex vacuo is an increasingly common cause of post-thora PTX in the ultrasound era. It is worth recognizing the illness script and understanding the physiology and mgmt
23/
24/24