See our qual exploration of clinicians in @PalliativeMed_j
liebertpub.com/doi/abs/10.108…
Care to take a stroll?
#pallipulm @pallipulm
@atscommunity
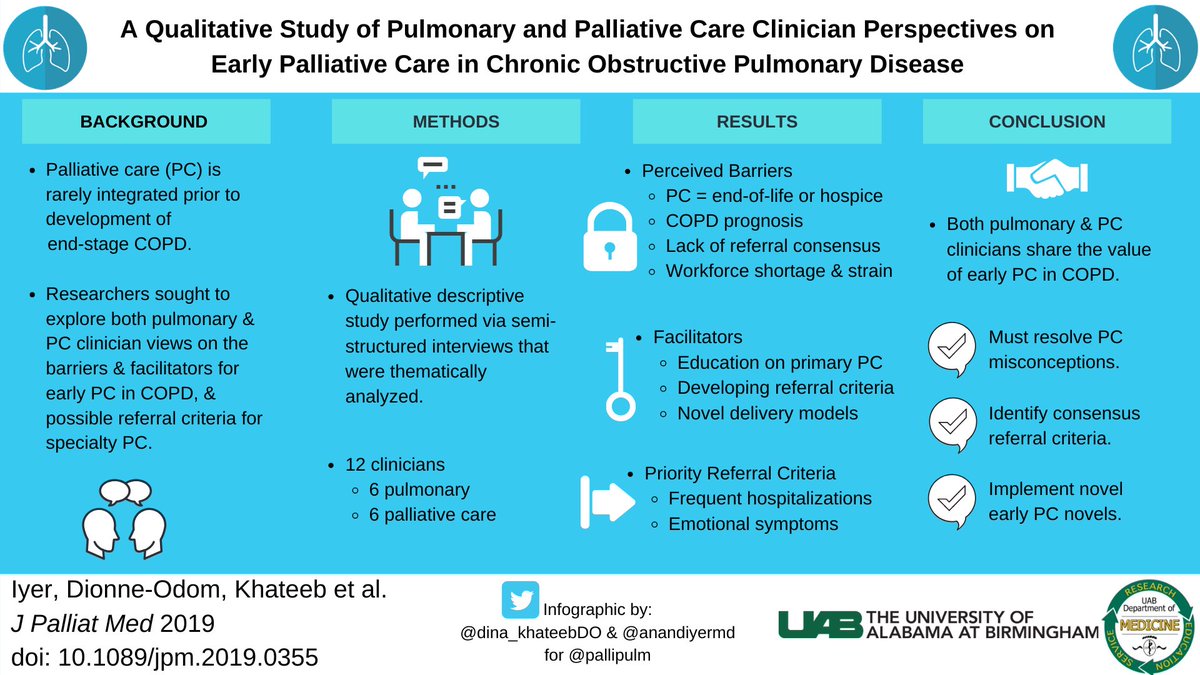
Waiting for PC until end-stage #copd is too late & misses a golden opportunity to meet COPD patient & family needs earlier in the trajectory.
See our @AnnalsATS pub atsjournals.org/doi/abs/10.151….
@AnnalsATS will have a podcast on that soon, so stay tuned!

Others have explored PC in COPD.
The key here is “early”.
Lots to learn from #qualitative research!
We identified themes on barriers to early integration/referral within broad educational, clinical, & operational categories & explored potential early referral criteria.
1) Not enough time in clinic for primary PC (this is a prob for everyone);
2) Inadequate reimbursement for primary PC (looking at you systems
@CMSGov)
3) Insufficient palliative workforce to handle COPD (@CTACorg @CAPCpalliative #pcheta)
1) More primary PC training in pulmonary (working on this through @atscommunity and @pallipulm)
2) Consensus referral criteria
3) Innovative delivery models, i.e. telehealth, nurse-led, embedded, etc.
Others were raised (oxygen, dyspnea, weight loss, pain, surprise question, etc).
These guide future work to move referral earlier. Symptom- or FEV1-based or both?
Thanks to @PalliativeMed_j & co-authors: @MBakitas @N_DionneOdomPhD @dina_khateebDO @realmdransfield
Comments?
@JoshFessel @KaminskiMed @ctsinclair @acderinger @kpedmonds @arifkamalmd @DianeEMeier











