I bet you are wondering, what's all the fuss with #candidemia? Why do we care? How to diagnose? How to treat?
Get ready for a thanksgiving treat!
Inspired by @DxRxEdu
In the US, invasive candidiasis is the most common fungal infection in hospitalized patients (4th most common infection overall)
1. C. diff
2. Staph aureus
3. E. Coli
4. Candida
www-nejm-org.proxy1.library.jhu.edu/doi/pdf/10.105…
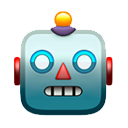
Here is a table summarizing the risk factors!
Some would include end-stage cirrhosis.
I feel that for some of these risk factors, you need more than one to be considered at increased risk, such as central lines, broad abx, colonization, etc
…k-springer-com.proxy1.library.jhu.edu/content/pdf/10…
There are no specific signs/symptoms to point us in the right direction. We have to think about the RF above and realize when a patient is not improving.
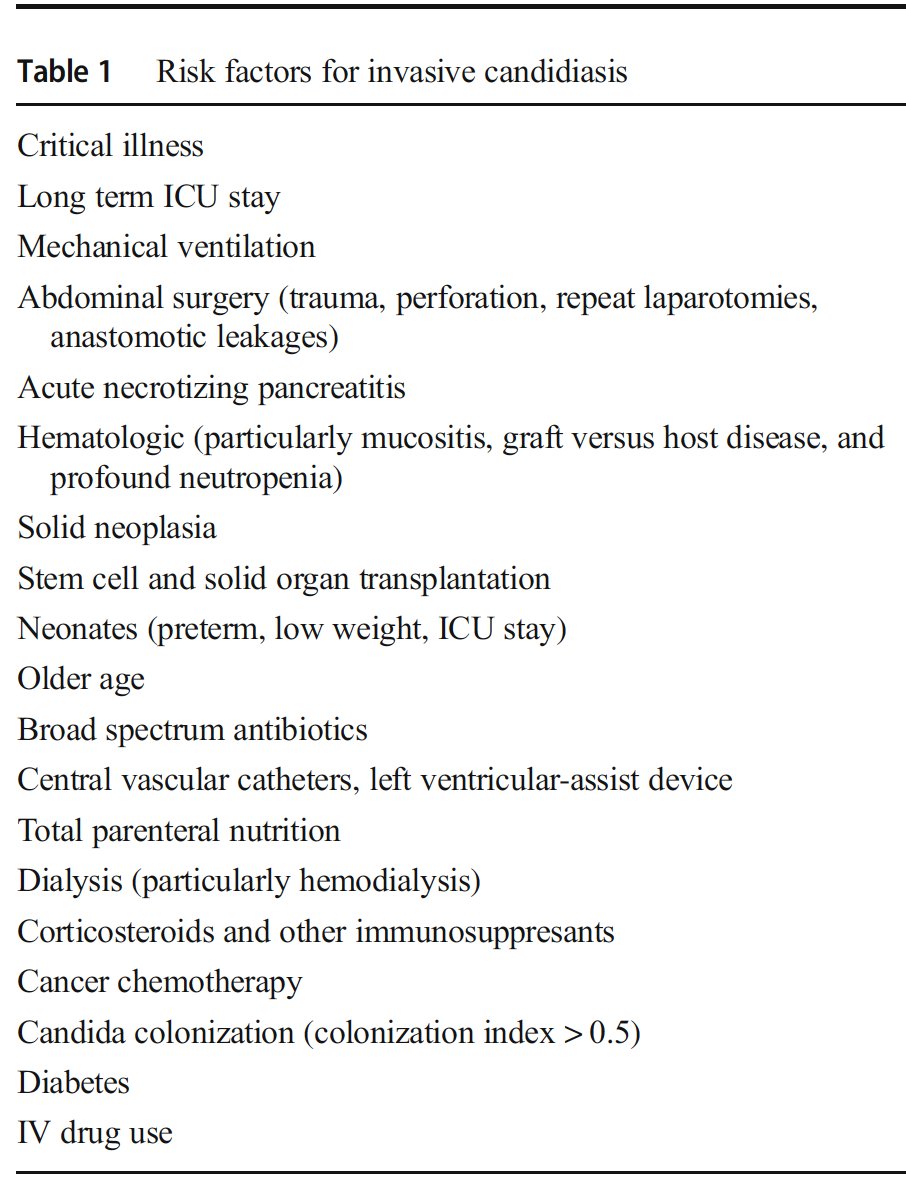
Mortality ⬆️2x with 12-24 hour delay in therapy 🤯
(table w/ fluc, more to come on therapy)
www-jstor-org.proxy1.library.jhu.edu/stable/pdf/448…
How to diagnose?
We should definitely be sending blood cultures (try for larger volumes if possible). Problem is that overall sensitivity is close to 50% 😰
Median time to positivity is 2-3 days!! Even more 😰😰
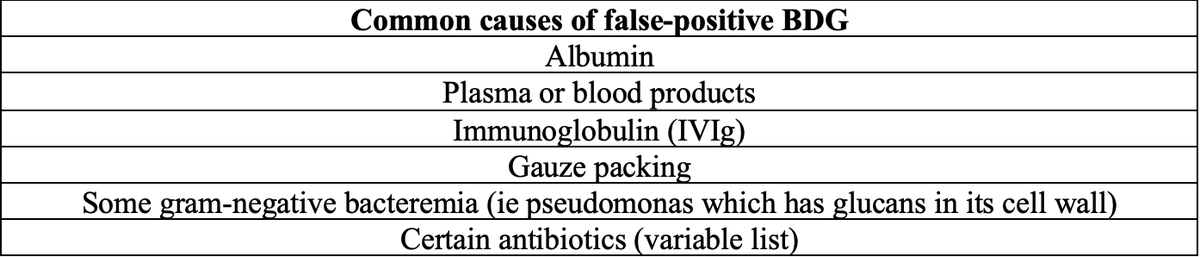
Should we be using beta-d-glucan (#BDG) to aid in the diagnosis of candidemia?
@GermHunterMD @ClancyNeil @DocWoc71 @ElliTheelPhD
What about T2Candida?
- T2 magnetic resonance to detect 5 sp (albicans, glabrata, tropicalis, parapsilosis, krusei)-appealing due to⬇️time to results, 3-5 hrs
Recent study, 68% candidemics +T2 test at day 0, ⬆️94% with serial testing @martinhoenigl
ncbi.nlm.nih.gov/pubmed/31613367
So, you get called in the morning because blood cultures sent from yesterday are now growing Candida sp, what do you start empirically?
@DrPappasID and others in the IDSA 2016 guidelines recommend an #echinocandin as first line.
Could use fluconazole if the patient is not ill or unlikely to have resistant organism, but that is hard to tell initially
academic.oup.com/cid/article/62…
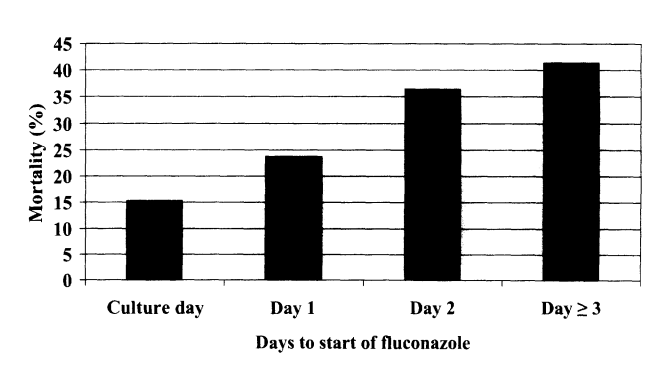
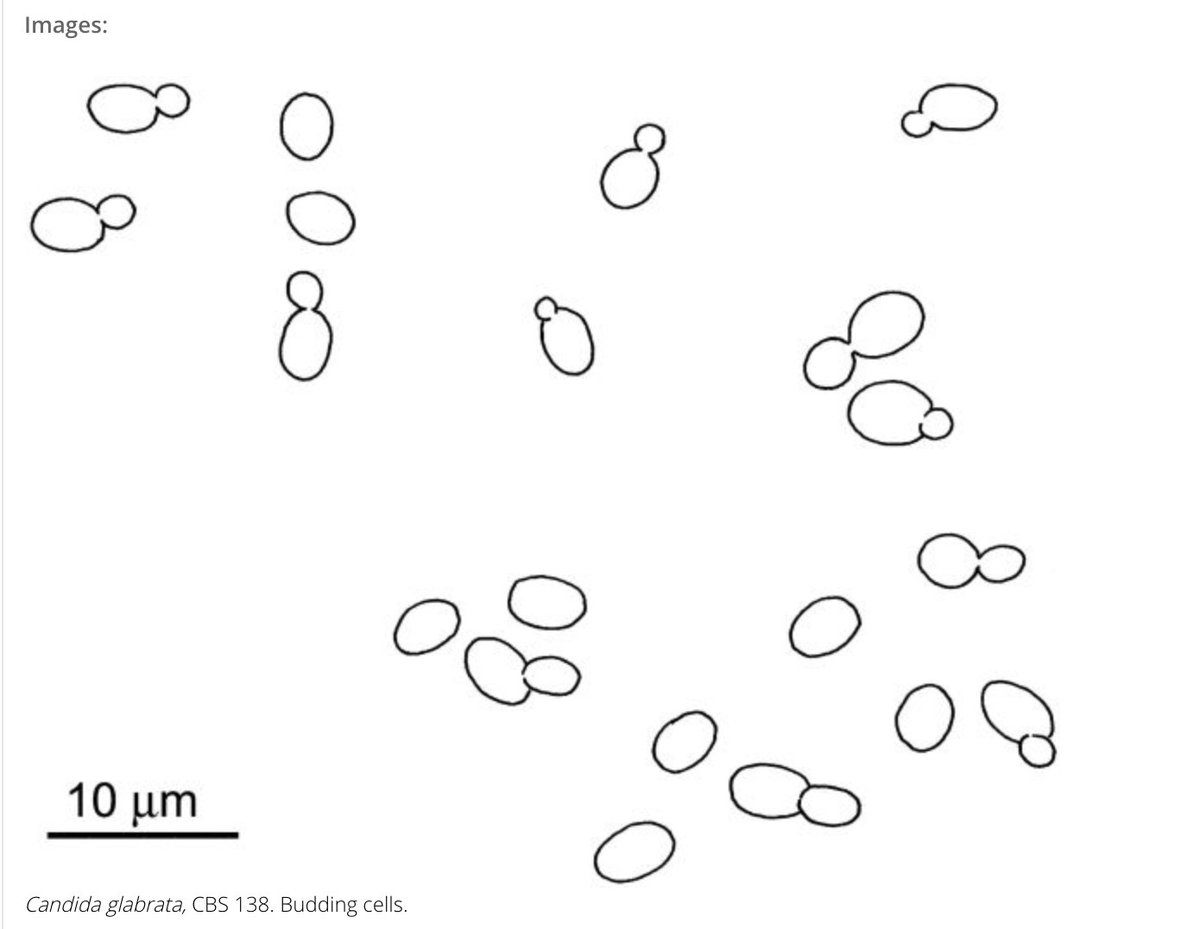
#IDDailyPearl for some of the Candida
- #albicans- most common
--can use fluc or echinocandin for bloodstream, may prefer one depending on clinical situation
- #glabrata- many are resistant to fluc
--seen more in elderly & cancer/SOT
images from clinicalfungi.org
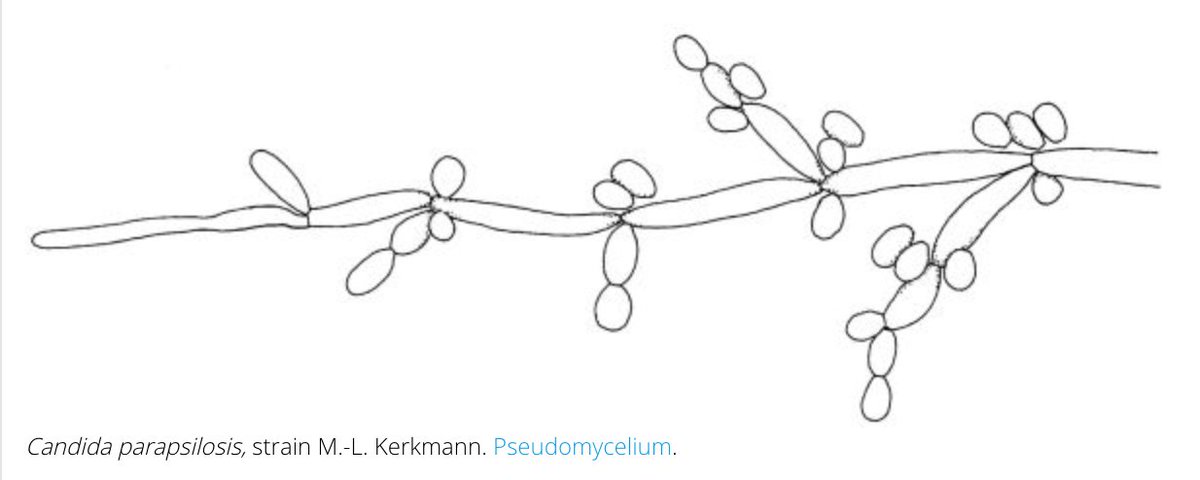
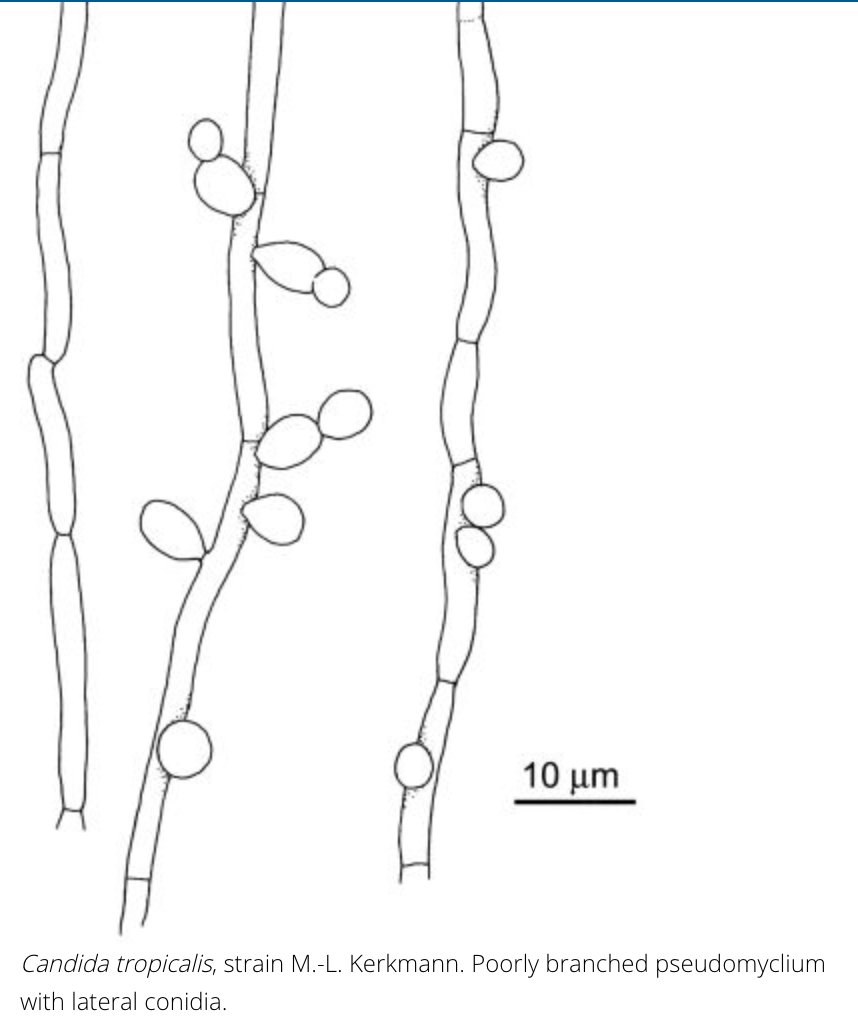
#IDDailyPearl
- #parapsilosis- biofilm on central lines
--can have higher MICs to echinocandins
- #tropicalis-⬆️freq in heme malig & stem cell tx
- #krusei-⬆️freq in immunodef & prolonged azole therapy --intrinsically resistant to fluc
images from clinicalfungi.org
I bet @andreaprinzi @Ahmed_HBabiker @richdavisphd @colleenkraftmd can provide more beautiful pictures and descriptions of the above!
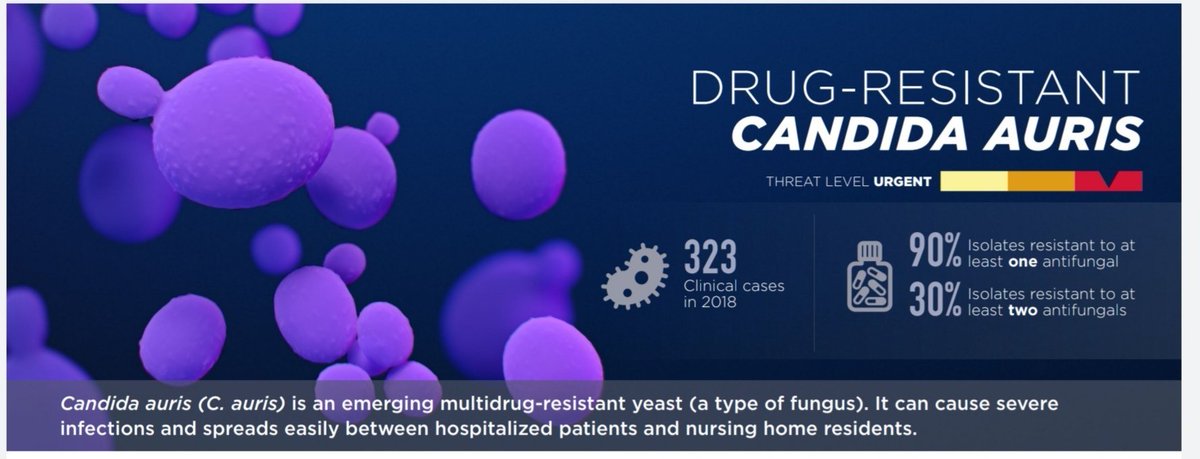
#IDDailyPearl
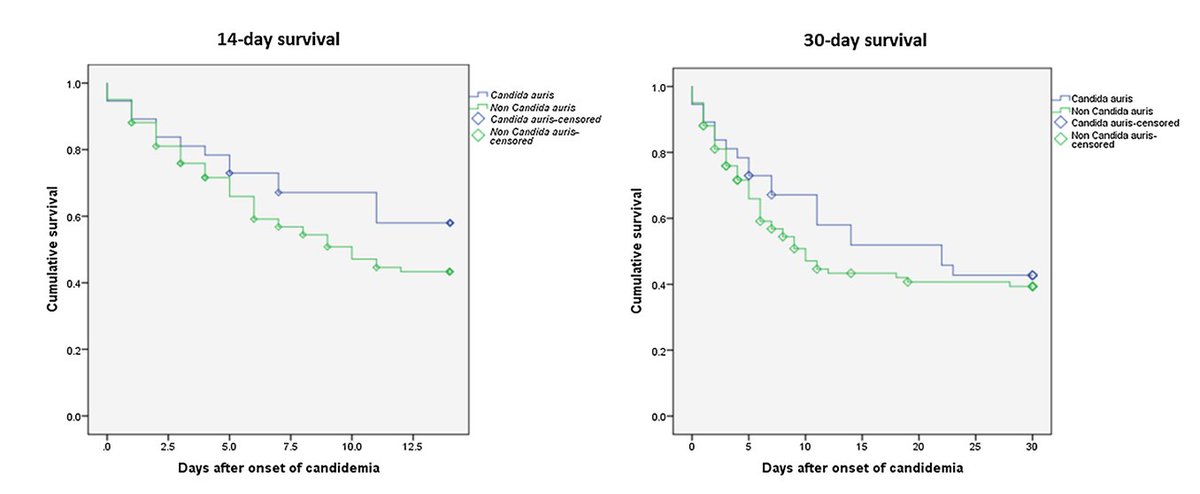
- #auris- lots of resistance...but does this confer increased mortality?
Several studies show NO increased mortality when compared to non-candida auris candidemia, including one published today!💥
@CDCgov released description below!
academic.oup.com/mmy/advance-ar…
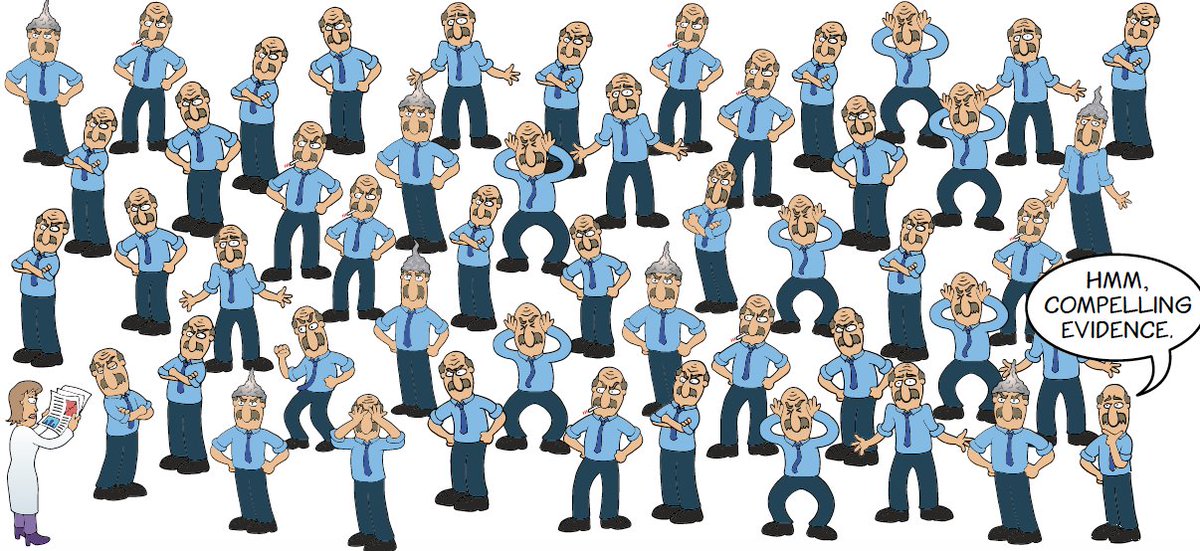
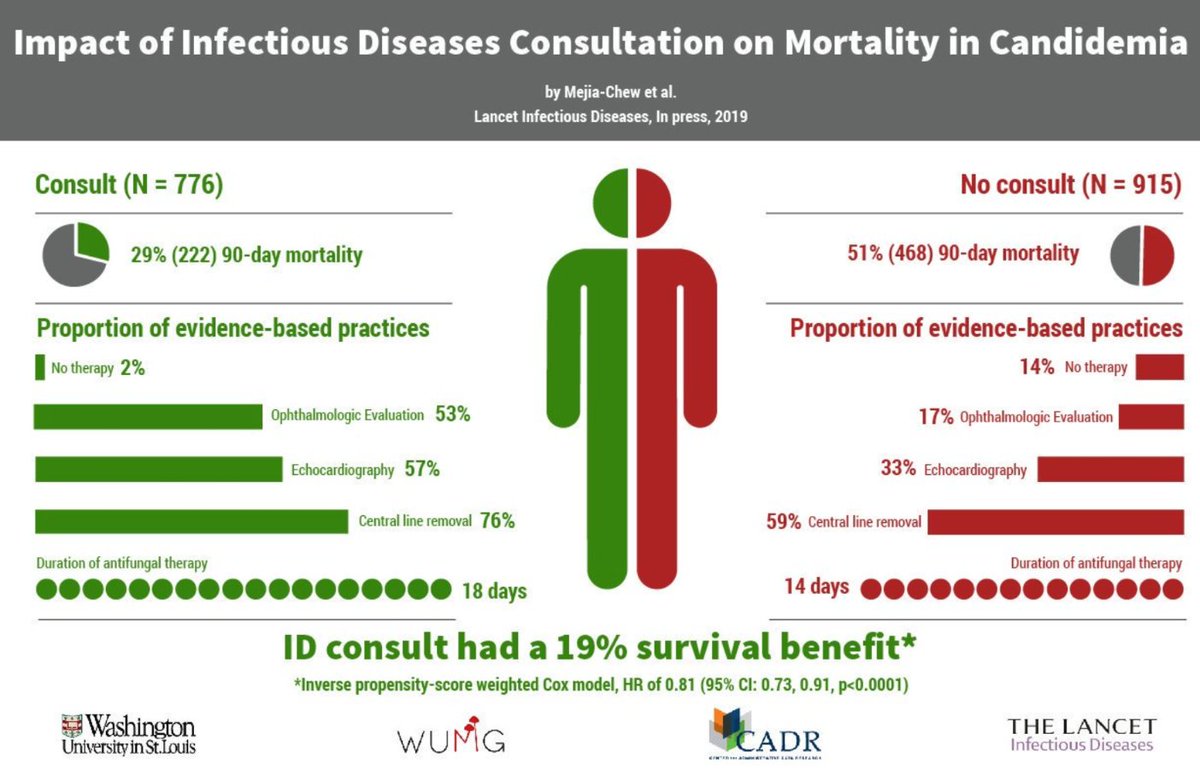
So, you get that call in the morning for candidemia. You know that time is of the essence - you start an echinocandin based on the IDSA guidelines you just read! Now, what do you do next to improve mortality?
@cmejiachew and @FungalDoc showed in @TheLancetInfDis that an ID consult improves mortality through the use of evidence-based practice:
- ophtho exams
- TTEs
- central line removals
- appropriate duration of therapy
ncbi.nlm.nih.gov/pubmed/31562024
To review:
- candidal infections are common in hospitalized patients
- there are RFs for candidemia (broad abx, ICU, central lines)
- high mortality & doubles quickly without therapy
- get blood cx
- start echinocandin
- get ID consult
Thank you, happy thanksgiving everyone