As @chrissyfarr notes, PF has become a bit of a cautionary tale. Perhaps there are useful lessons in that tale. 1/n
From what I can glean via purely public info, the opioid episode seems to have happened in late 2016 and 2017.
I.e. that cloud-based EHRs could help transform a fragmented care delivery landscape into a connected clinical community, while generating useful data for research/RWE.
Specifically, in 2014/15, PF worked with Merck to develop workflow tools based on CDC guidelines that would try to boost pneumococcal vaccination in the elderly.
That campaign was reported at the time, in a largely positive light, and Merck's role was transparent:
forbes.com/sites/zinamouk…
Obviously, Merck funded the work to sell more vaccine doses. On the other hand, channeling pharma resources in this way can serve public health - there are similar "uptake" incentives in some Hep C treatment contracts.
FWIW, I also don't think "hindsight" claims are an excuse - Sam Quinones's "Dreamland" came out in 2015, and Meier's "Pain Killer" years before.
And - at least in this case - the program does not seem to have explicitly nudged physicians to prescribe pain meds, only to document a pain score.
Most likely, nudging an MD to document pain boosts the propensity to prescribe pain pills. Just like those "talk to your doctor about X" ads.
It is harder to build a business focused on clinical quality or patient value than to milk the status quo. But once established, revenue models take on a life and logic of their own. Please choose carefully.
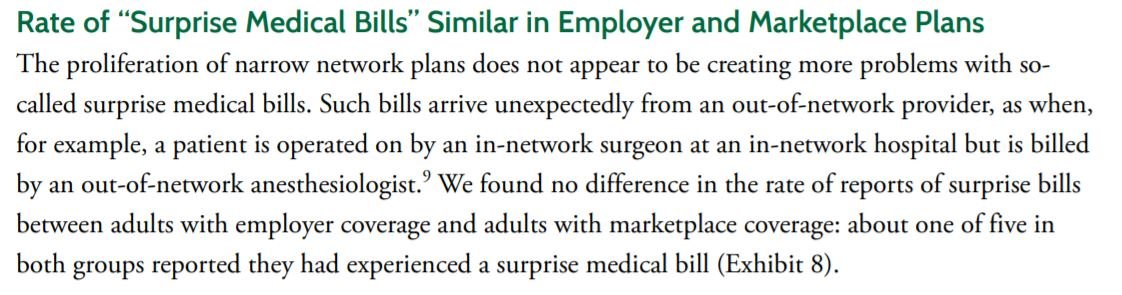
True of surprise billing, extractive hospital collections, and Valeant-style abusive drug pricing. And it sure as hell is wrong to push addictive pills through an EHR. /n