Now that I've read it, I wonder—quite sincerely—how this article got past peer review.
This is not a tenable assumption. The RAND HIE is dated, but it's not obsolete—it's backed up by a whole canon of health economics research now.
The best relevant evidence we have (from Oregon's randomized Medicaid expansion) is that coverage actually increases use of the ED, including for nonemergent care.
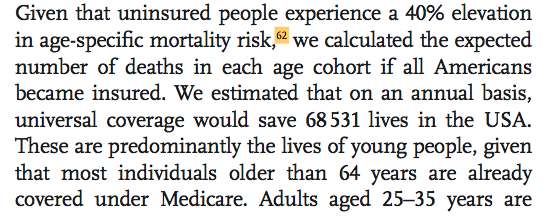
However, to reach their top-line number (68,531 lives saved annually) the authors rely on a single paper from 2009. ncbi.nlm.nih.gov/pmc/articles/P…
Medicaid expansion, generally: www-personal.umich.edu/~mille/ACAMort…
For ESRD patients specifically: jamanetwork.com/journals/jama/…
But we're still going to have issues related to, for example, interoperability of EHRs—perhaps even more so when there are no networks hemming people into shared HIT ecosystems.
MedPAC says hospitals had an aggregate Medicare margin of -9.9% in 2017. medpac.gov/docs/default-s…
This debate is important, and we're going to be having it for a long time yet. It's important that evidence put forward in service of this debate can stand up to rigorous evaluation.
And if these constraints *are* binding, it's going to erode the purported mortality and health benefits of coverage expansion.
I also think that hospitals will find ways to change supply inputs to eke out those extra margins over the medium and long-term.