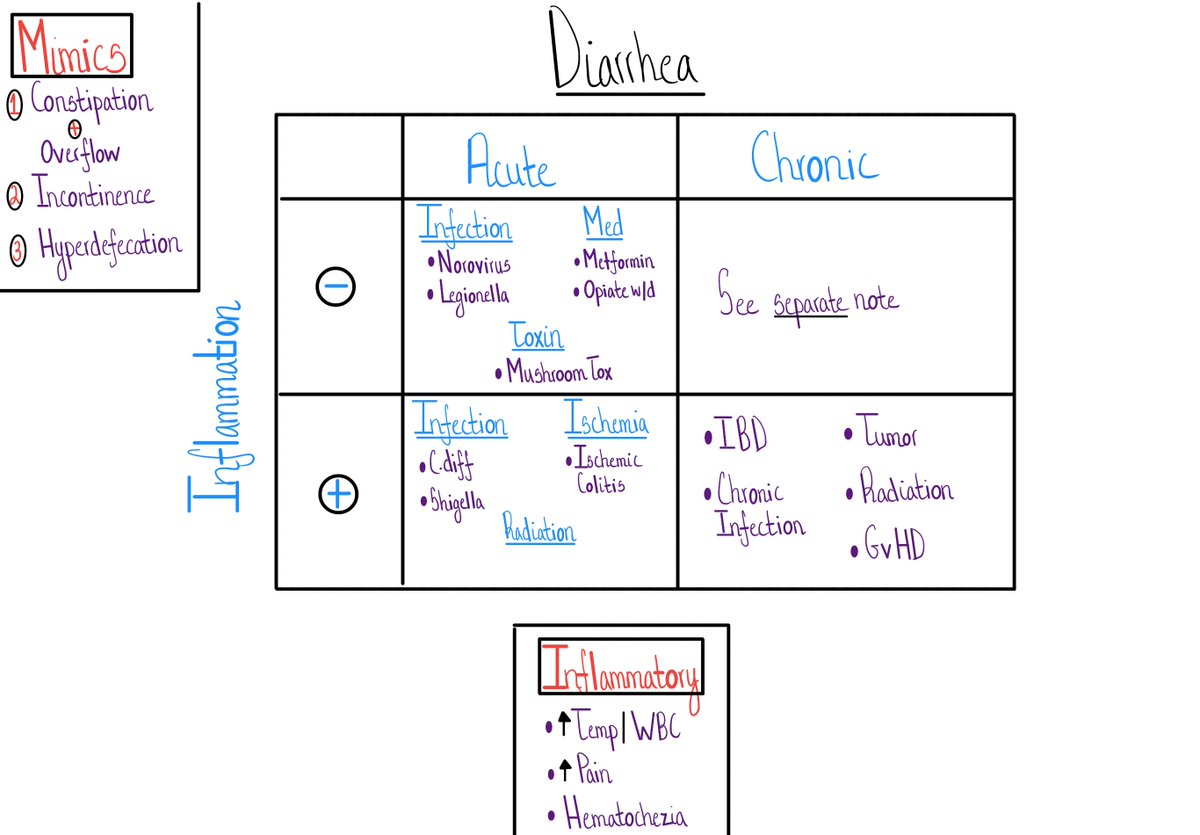
Diarrhea - Part 1
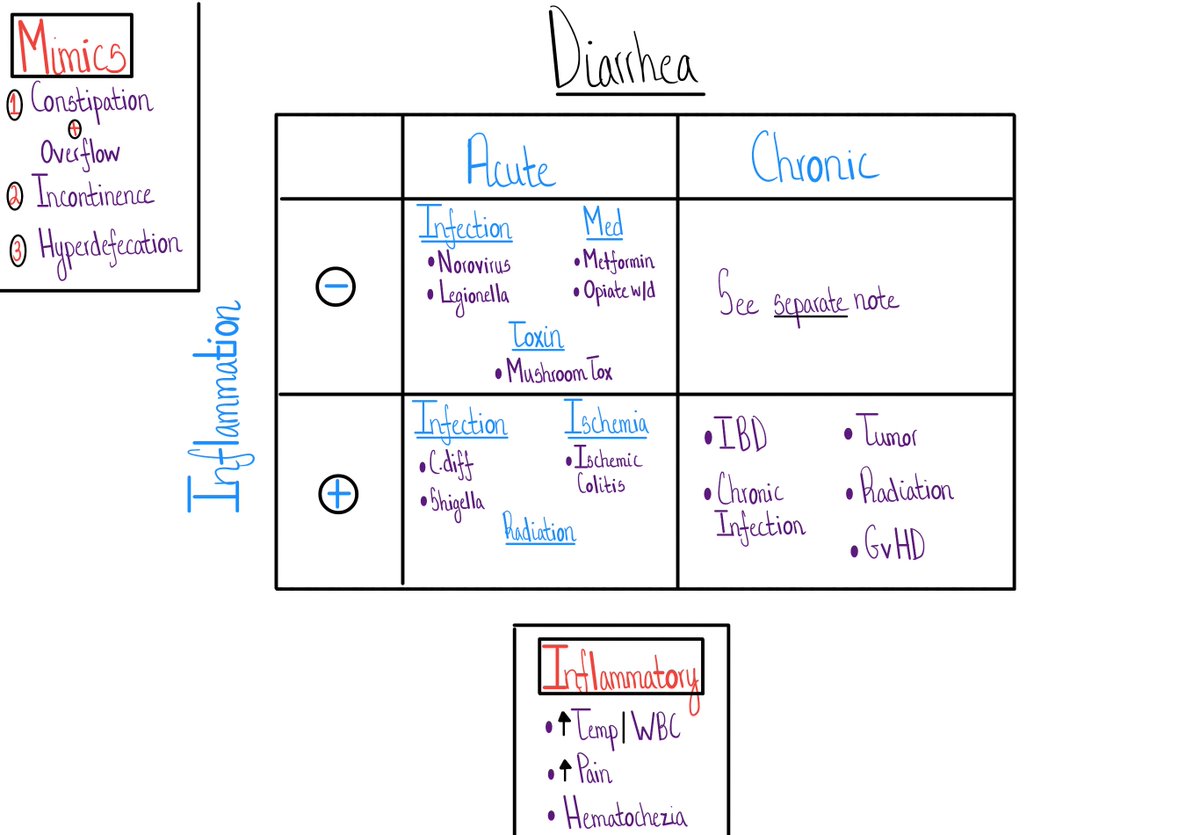
3 Misleading Mimics
&
2 Key Questions
Join us #medtwitter & #medstudenttwitter
We tend to use the term loosely (Ha! 😉) so your patient may be referring to another change in bowel habits when they say diarrhea.
How do we know?
The Bristol Stool Chart!
bit.ly/2TWeVgS
🙏🙏 @Dietitianbytes
1. Constipation + overflow
2. Stool incontinence
3. Hyperdefecation
This amazing @COREIMpodcast case is a great example - bit.ly/332uDuR
I've been fooled by all 3...multiple times.

If you are confident your patient has diarrhea, 2 pieces of data organize what is an incredibly long DDx.
1. Time course - acute (<2-4 weeks) or chronic (>2-4 wks)
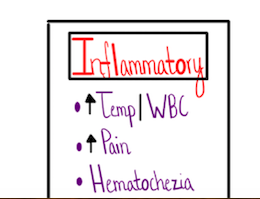
2. Inflammation
I am so glad you asked!
Determining "inflammation" in general - bit.ly/2VXeky0
There are other, more advanced, methods too, like the fecal calprotectin - bit.ly/38DW6UK
Notice how we've simplified the mechanism from -
Osmotic, Secretory, Inflammatory
to
Non-inflammatory & Inflammatory.
The DDx of ACUTE diarrhea is limited enough, that the extra cognitive energy to classify as osmotic versus secretory isn't worth it.
Chronic diarrhea is a whole different equation.
We'll talk about that soon.
Yes!
A reasonable # of extra-intestinal infections result in acute diarrhea
🤯🤯🤯
More here - go.nature.com/2Iz6nXI
Yup - infections make it on both lists - inflammatory and non-inflammatory acute diarrhea
We don't need a specific microbiologic Dx for most acute infectious diarrhea - a large # is viral - but key your eye out for:
2. Traveler's diarrhea - a large fraction is bacterial
(the majority don't need antibiotics)
Great review from @adamcifu here - bit.ly/2TAtmIp
4. Most patients with acute infectious diarrhea outside C.diff, don't need antibiotics.