Can #SARSCoV2 #variants fully evade #vaccine induced protection? Or even natural protection?
The rapid emergence of too many different #variants shows that the virus is struggling to survive! That is why it’s changing so fast, probably, to prolong its stay in human bodies 1/
The rapid emergence of too many different #variants shows that the virus is struggling to survive! That is why it’s changing so fast, probably, to prolong its stay in human bodies 1/
Though #vaccines may not be working perfectly against some #VOCs, but those fully vaccinated are protected against severe disease & death. No VOC can completely evade the vaccine induced protection, especially against severe disease & death! Why?.......... 2/ 



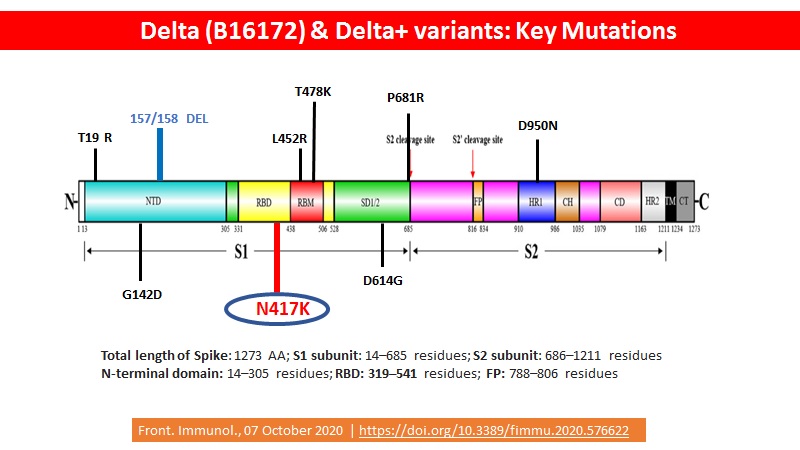
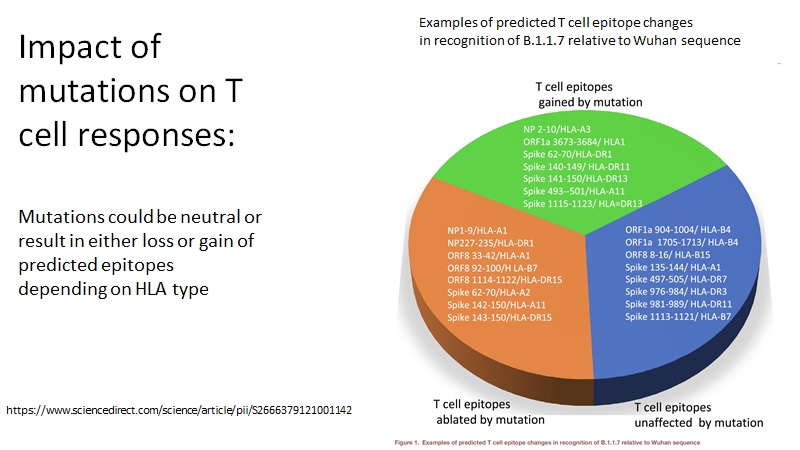
The #variants do not have changes in T-cell epitopes because when you are infected with a variant that evades an antibody, that variant can go to someone else and evade their antibody too. So it spreads through the population.... 3/
But, if you have a variant that evades a T-cell, it is not going to make a difference in the next person because everybody's T-cell #epitopes are different. And so, T-cell variants of viruses generally take many, many, many years to emerge. May be decades? 4/
Further, there are many many more T cells epitopes than of B cells. With fine-mapping of #Spike T cell epitopes very much still ongoing, around 280 #CD4 epitopes have already been identified & many more of #CD8 5/
While some 450 #CD8 epitopes have been described across #HLAI alleles, recognition of only very few of these would be impaired (for some alleles) in an individual primed by natural infection or vaccination to the wild-type virus & then encountering the variant 6/
An additional twist: T cell #epitopes may be gained, lost, or unchanged in a variant compared to original sequence virus. So, there may be even gain of additional T cells epitopes 7/ 
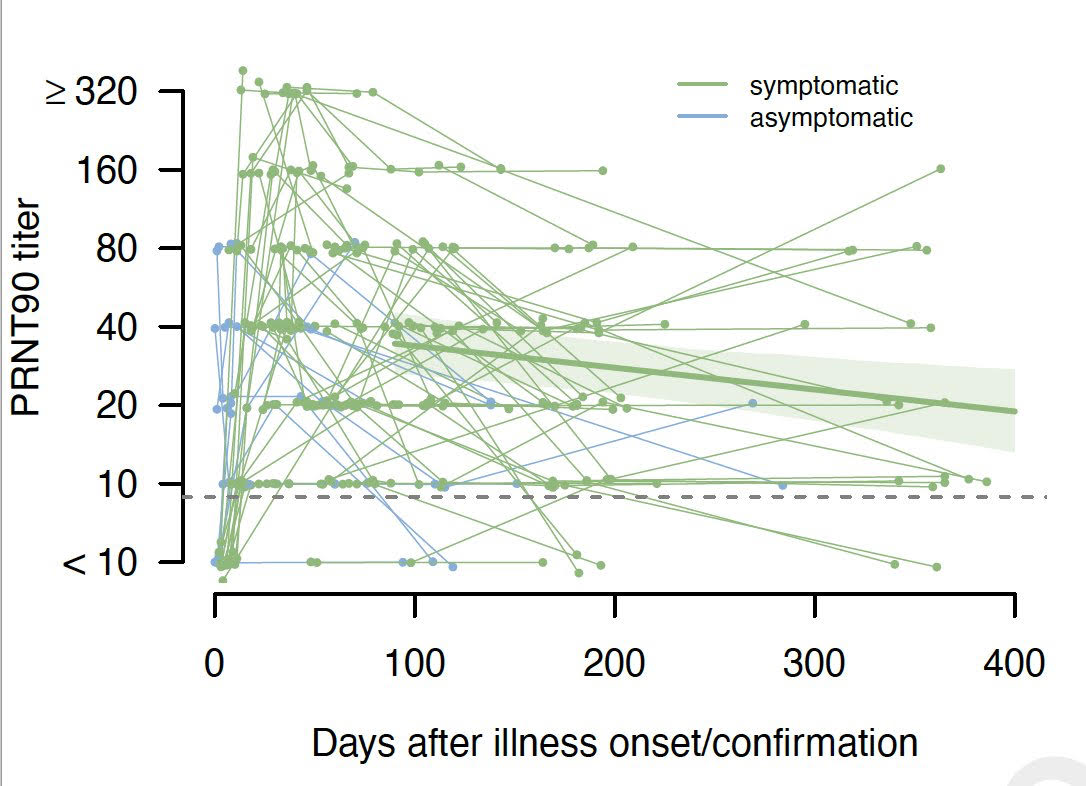
While most attention on likely 'correlates of protection' centers on #NAbs titer and, to a lesser extent, on #CD4 T cell response, it is likely that #CD8 immunity is important, and this response is strongly correlated with the antiviral CD4 response 8/
There are many people who have #activated T cells & no #antibodies, as people who have antibodies. It is unclear how many of those people with activated T cells and no antibodies actually have immunity. But it is difficult to make some guess in terms of percentage 9/
Are the antibodies totally redundant? No, you see influenza virus T cells are also important, yet when the virus changes its B-cell epitopes, we decide to change the vaccine. It means antibodies do contribute 10/
Antibodies prevent infection, not T-cells. They help in attenuation of the disease & prevent death. Even though my T-cells are great, I still want to have some antibodies. So, the two work together. 11/
Hence, the T-cell immunity is the last defense against an infection....can protect a lot of people in the face of even low Ab response. Some agammaglobulinemic people who don't make Abs but they don't have an unusually severe course, because the T cells are protecting them 12/
• • •
Missing some Tweet in this thread? You can try to
force a refresh