Why does nephrotic syndrome (NS) present with periorbital edema?
I generally feel comfortable explaining why patients with NS have edema. But, why does it accumulate around the eyes? And, why doesn’t heart failure present this way?
Time for more Starling! And George Burch...
There are at least three things that help to explain periorbital edema in nephrotic syndrome:
*rapidity of edema onset
*anatomy of the eyelids
*the “lesion” in the Starling equation
Certain types of nephrotic syndrome (e.g., minimal change disease) are associated with rapid protein loss. This contributes to edema formation over a period of days to a week.
Is there another form of edema that is even more rapid onset (hyper-acute)?
Of course there is…
…angioedema! And this also presents with periorbital edema. So, maybe this is a clue.
There is something about the eyelids that “allows” for rapid fluid accumulation in both angioedema and NS.
Which of the following does the periorbital space contain a lot of?
Eyelids contain lots of loose connective tissue which typically have negative interstitial pressures (e.g., -3mmHg).
This may be part of it.
But, there is low compliance at negative pressures (i.e., pressures increase a lot even with little edema).
physiology.org/doi/10.1152/ph…
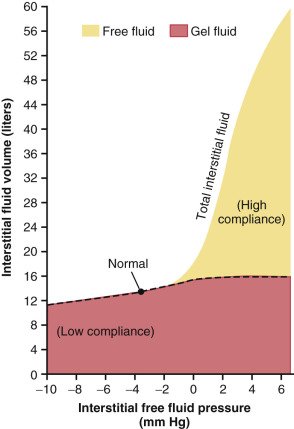
There must be something else.
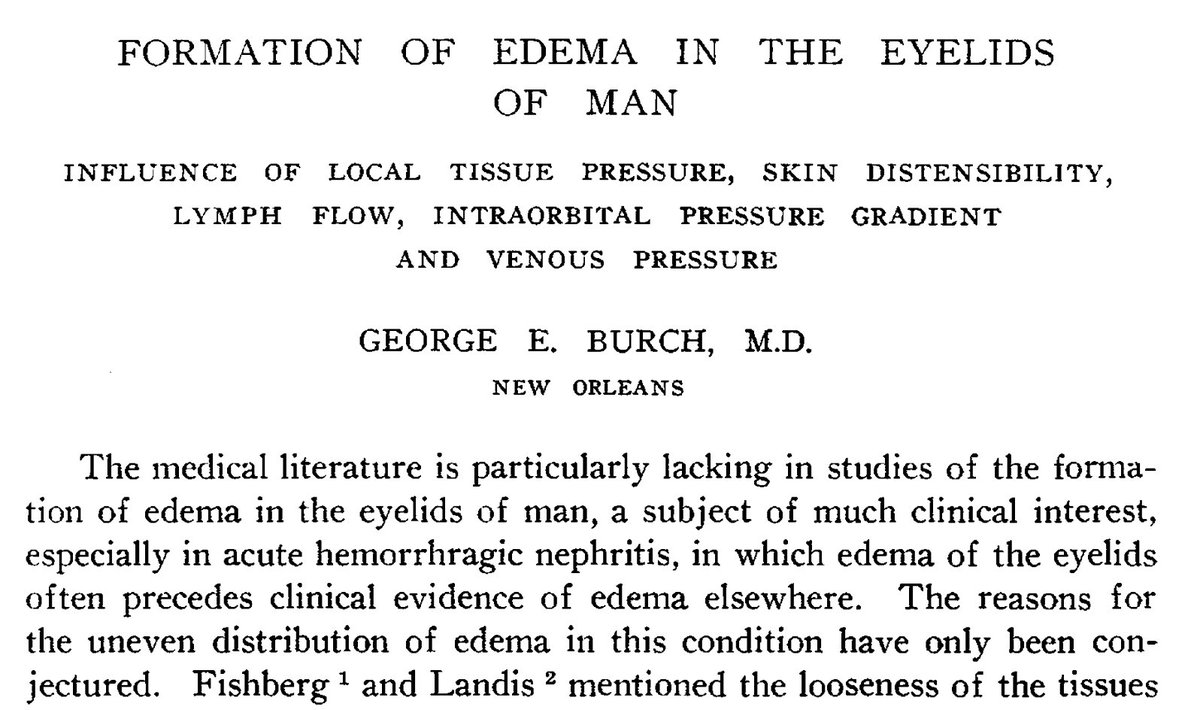
Amazingly, George Burch was bothered by this, more than 90 years ago. What did he do: lots of experiments, with results published in an awesome 1940 Archives of Internal Medicine paper.
jamanetwork.com/journals/jamai…
Interim summary:
*periorbital (eyelid) edema may occur when fluid accumulation is rapid onset
*some forms of nephrotic syndrome are rapid onset
*the loose connective tissue and distensibility of the periorbital space likely contribute to their being involved
In angioedema and nephrotic syndrome, the acute changes in the Starling Equation (allowing for rapid onset edema) are different:
*angioedema = increased capillary permeability
*nephrotic syndrome = decreased plasma oncotic pressure (note: edema in NS if multifactorial!)
Early on, these changes lead to edema in locations conducive to rapid accumulation of interstitial fluid. Spaces like the eyelids.
In nephrotic syndrome, patients may subsequently experience generalized edema. The mechanism for this is different (e.g., #15-16 below).
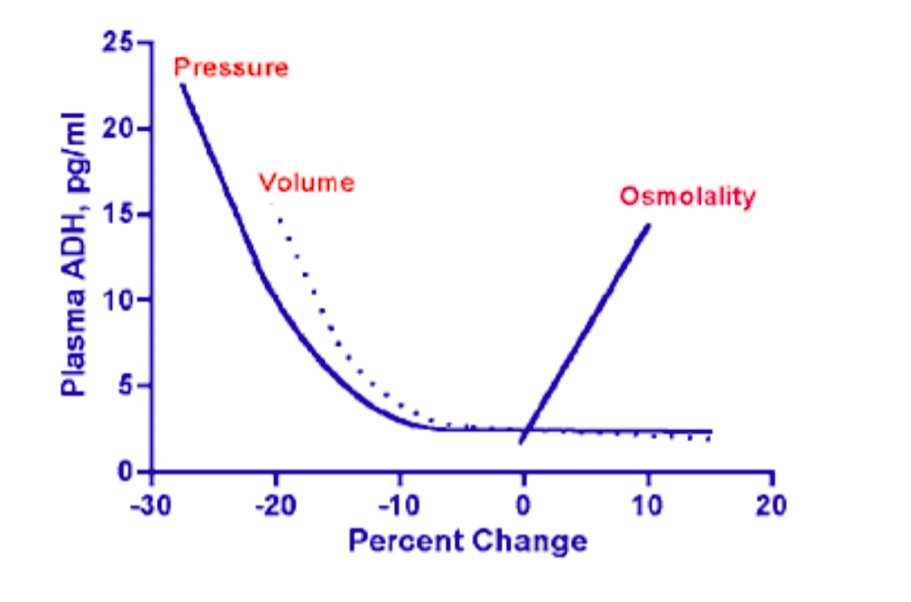
Mmmm, can acute edema be related to an abrupt change in capillary hydrostatic pressure (Pc)?
Absolutely! We see rapid increases in Pc in acute DVT and acute pulmonary edema.
Notice that these lead to localized edema where the Pc increased.
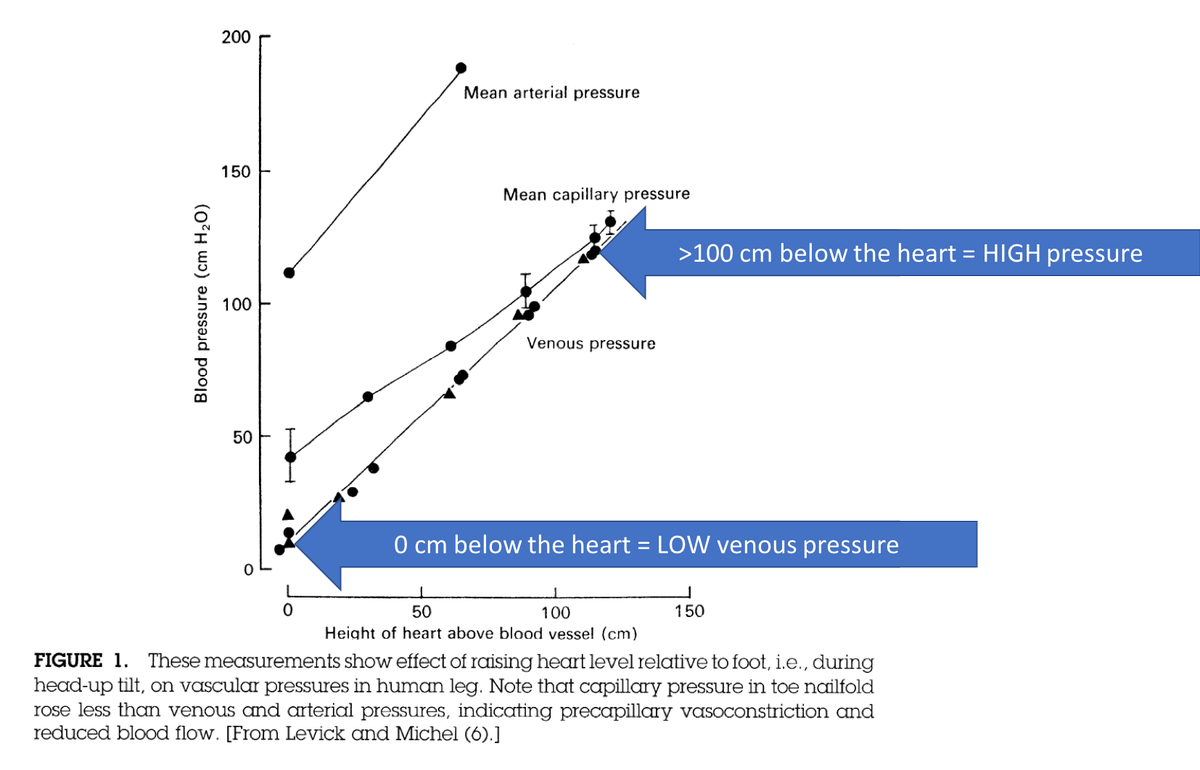
In chronic heart failure, the elevated Pc is greatest in dependent locations, as the pressures are higher due to the effects of gravity.
This is why we often see edema in the feet and not in the face.
physiology.org/doi/10.1152/ph…
Before ending this thread, it’s important to say that the etiology of edema in nephrotic syndrome is multifactorial and likely differs from patient to patient.
I want to highlight one fascinating mechanism, recently identified.
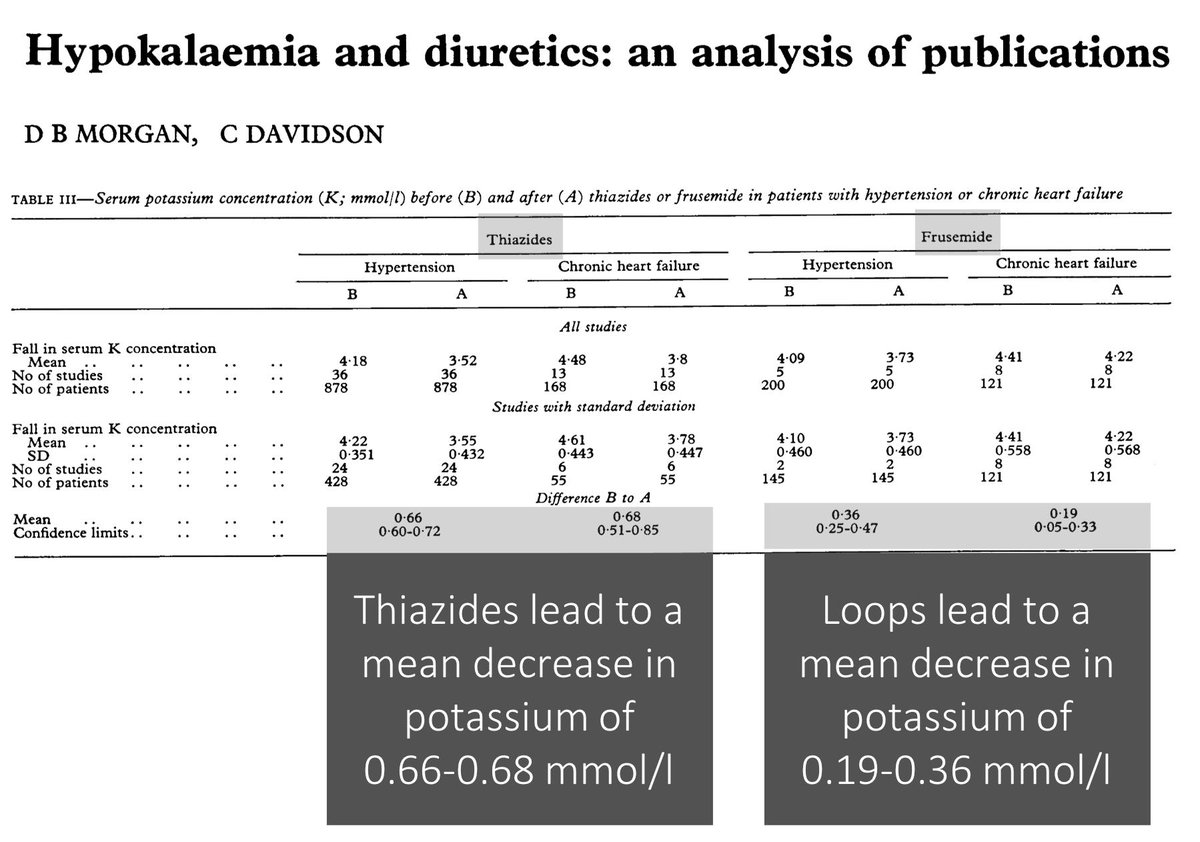
Sodium retention is a likely contributor in many patients. But why does nephrotic syndrome lead to sodium retention? When explaining this in the past, I hand-waved the usual decreased-renal-perfusion-elevated-RAAS mechanism.
This is part of the “underfill” hypothesis.
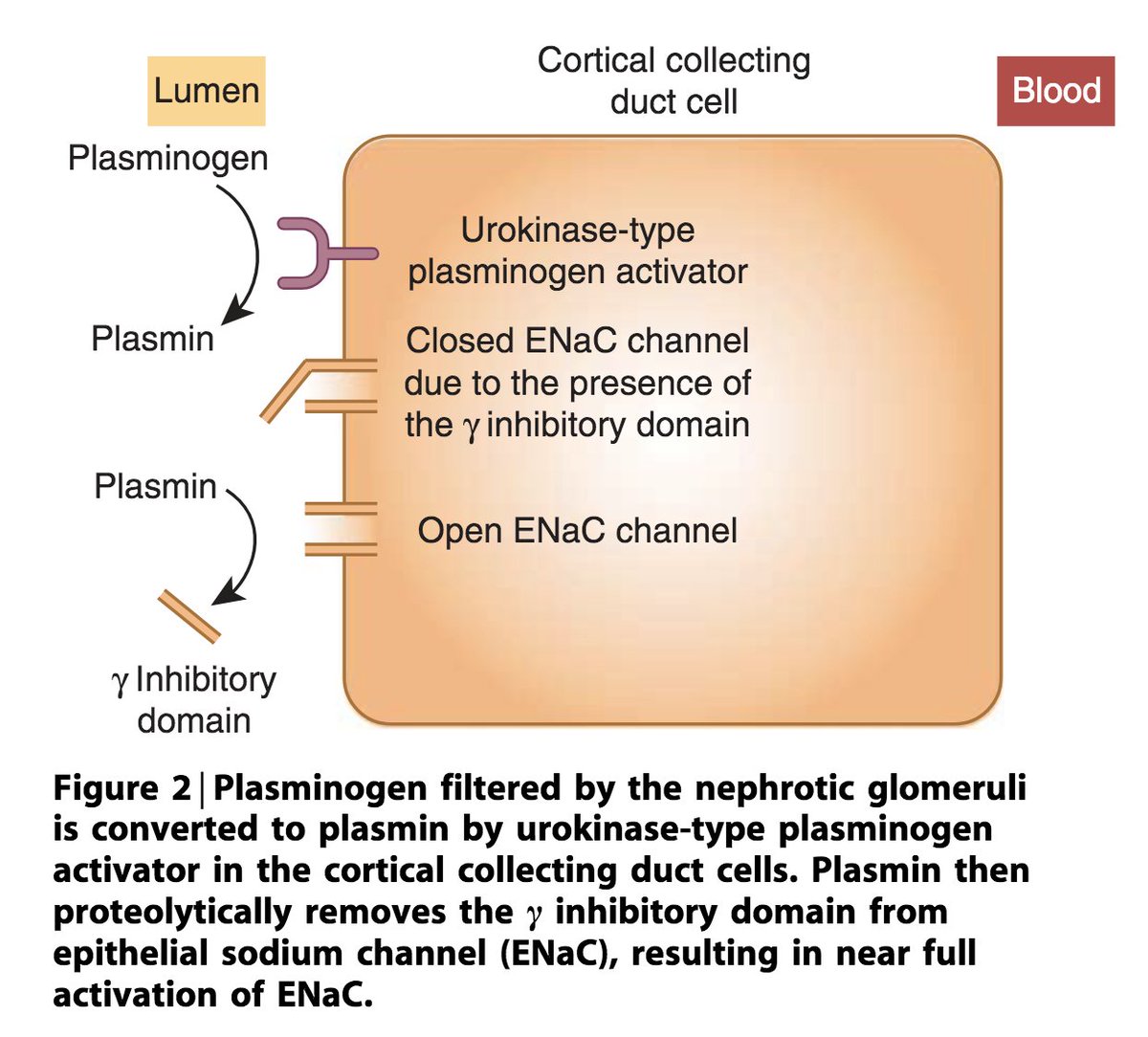
Amazing research has shown:
*increased filtration of plasminogen, leading to
*cleavage of the gamma chain of the epithelial Na channel (ENaC) in the DCT, leading to
*increased activity of the ENaC, leading to
*increased Na retention
So cool!
linkinghub.elsevier.com/retrieve/pii/S…
In summary, the periortibal edema seen in NS likely occurs:
*when protein loss is rapid
*as a result of the special compliance of eyelids to rapid fluid accumulation
And:
*more generally, edema in NS is multifactorial
*plasmin mediated activation of ENaC may contribute
I'm very curious how others (e.g., @kidney_boy @Nephro_Sparks) think through this. It's hard to find articles directly addressing this exact question...