Two questions to start.
First, which of the following is the major mechanism by which pulmonary embolism leads to hypoxia?
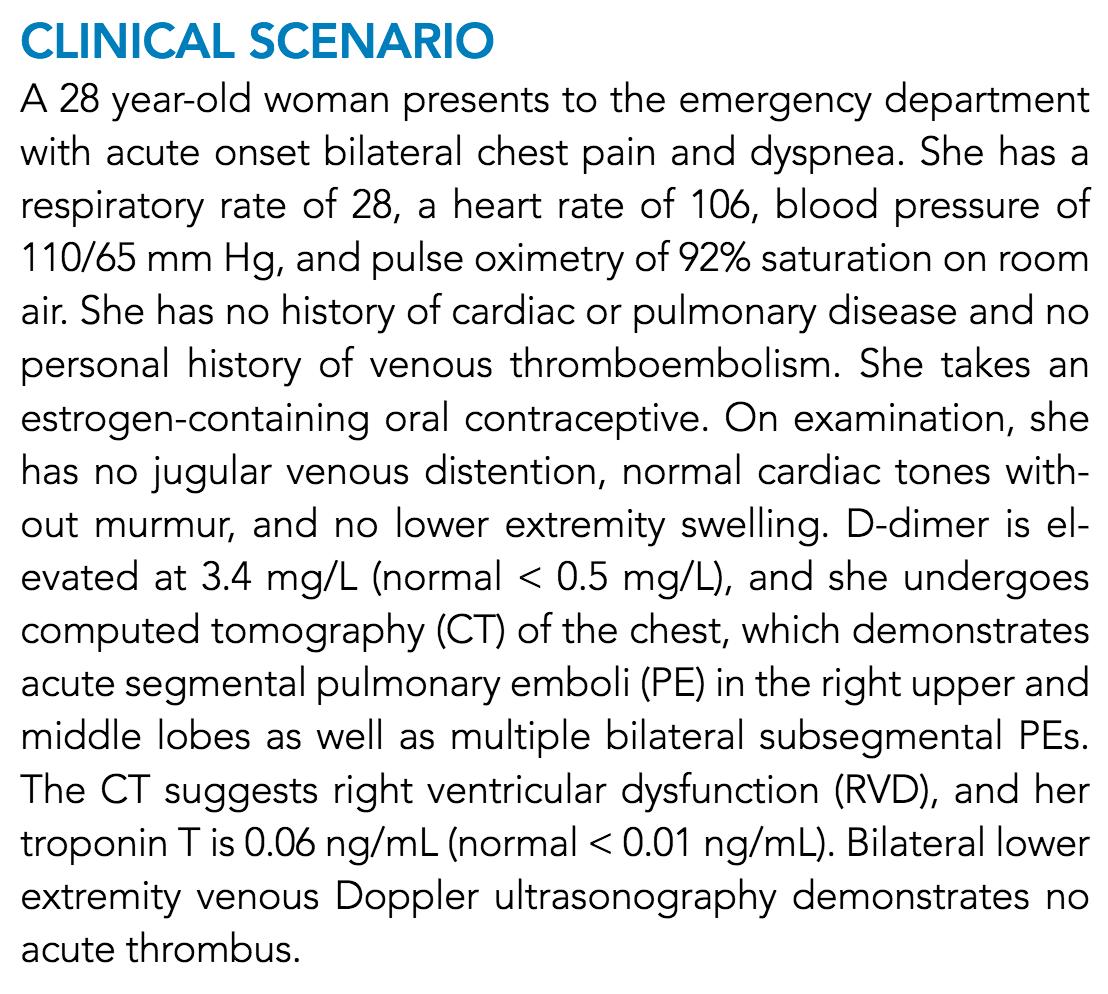
Acute PE leads to hypoxia primarily via V/Q mismatch. But, what's altered? And, in what direction?
[V=ventilation; Q=perfusion]
While PE surely causes decreased Q, this leads to deadspace ventilation (i.e., areas of V but no Q). Deadspace ventilation does not cause hypoxia.
So, although decreased Q occurs, it's not the answer.
What is the cause? INCREASED Q! Let's see how.
ncbi.nlm.nih.gov/pubmed/25006441
Two clues that the mechanism isn't related to the thrombus itself (i.e., decreased Q):
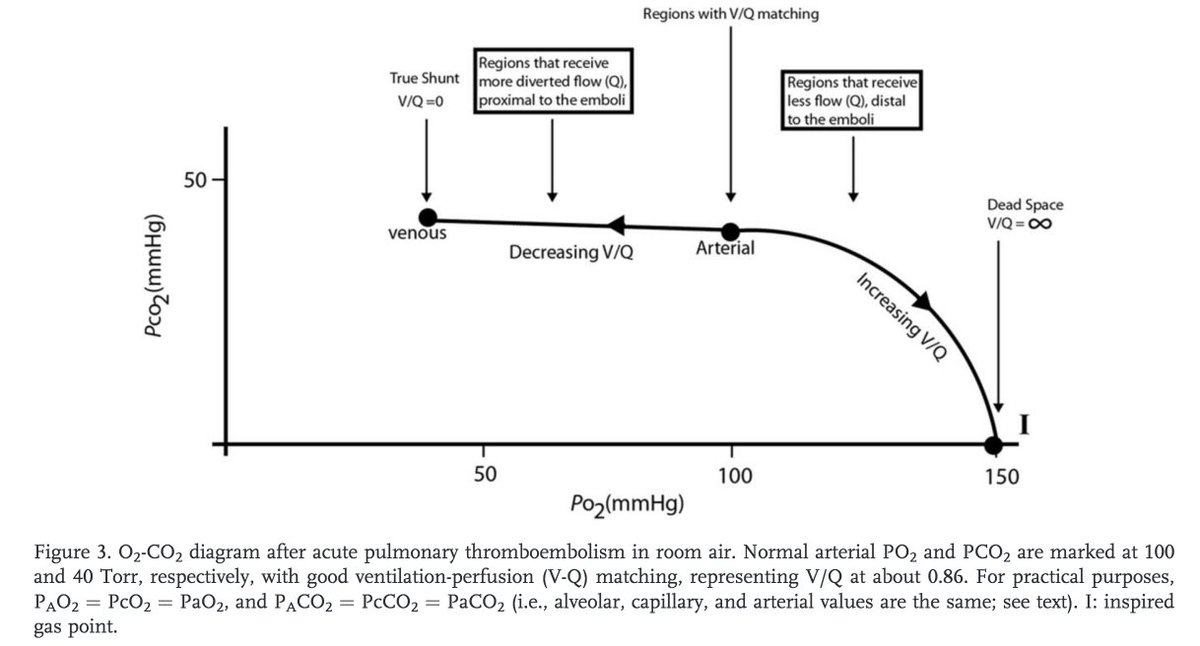
1. PaO2 varies widely, even in those with large PEs (Pic/Study 1)
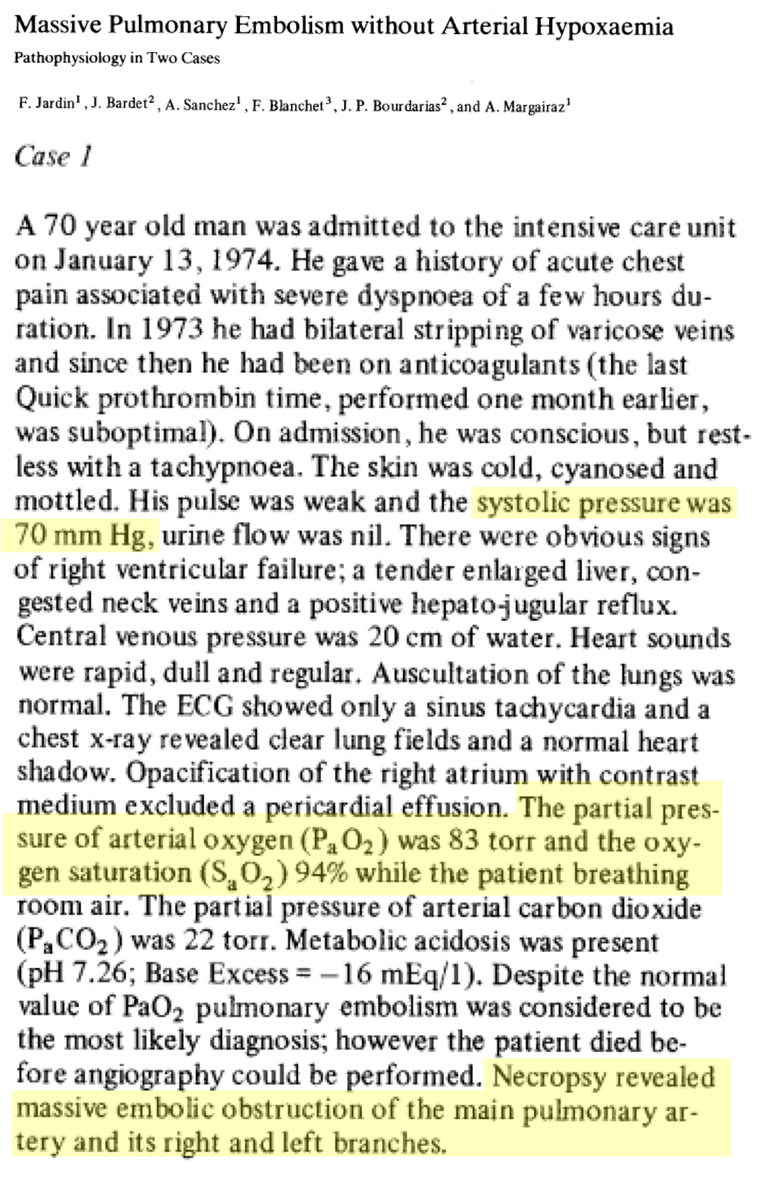
2. some patients with massive PE don't even have hypoxia (Pic/Study 2)
ncbi.nlm.nih.gov/pubmed/4266893
ncbi.nlm.nih.gov/pubmed/893777
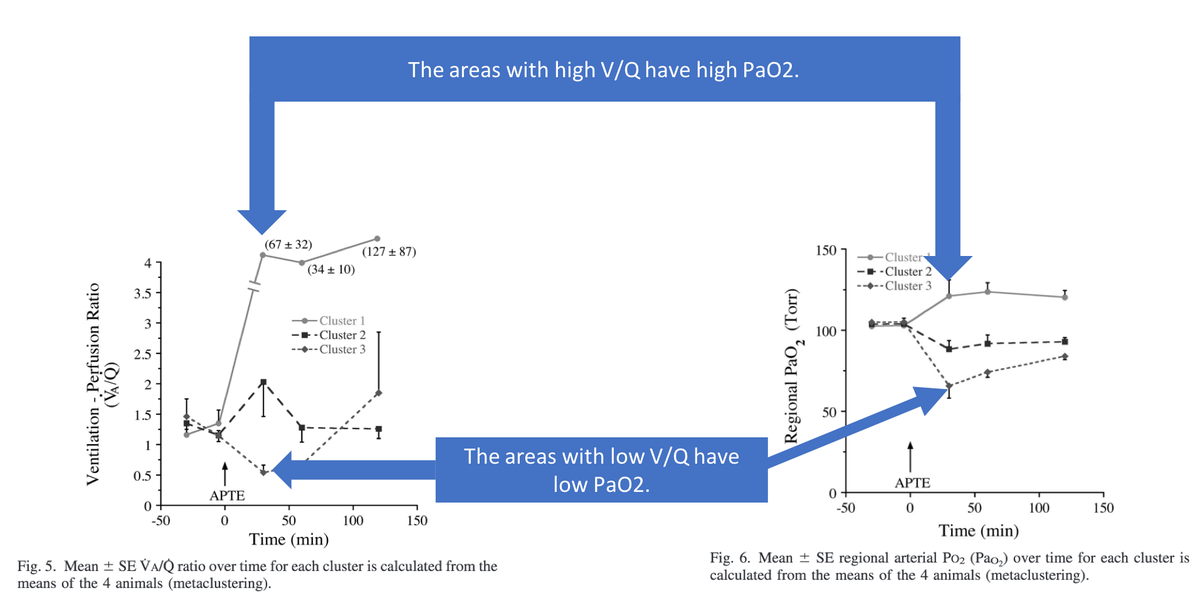
Something is happening away from the clot. In acute PE, there are two key areas of the lung:
1. High V/Q (i.e., deadspace). These are the areas affected by the clot.
2. Low V/Q. These are the areas NOT affected by the clot.
ncbi.nlm.nih.gov/pubmed/15591291
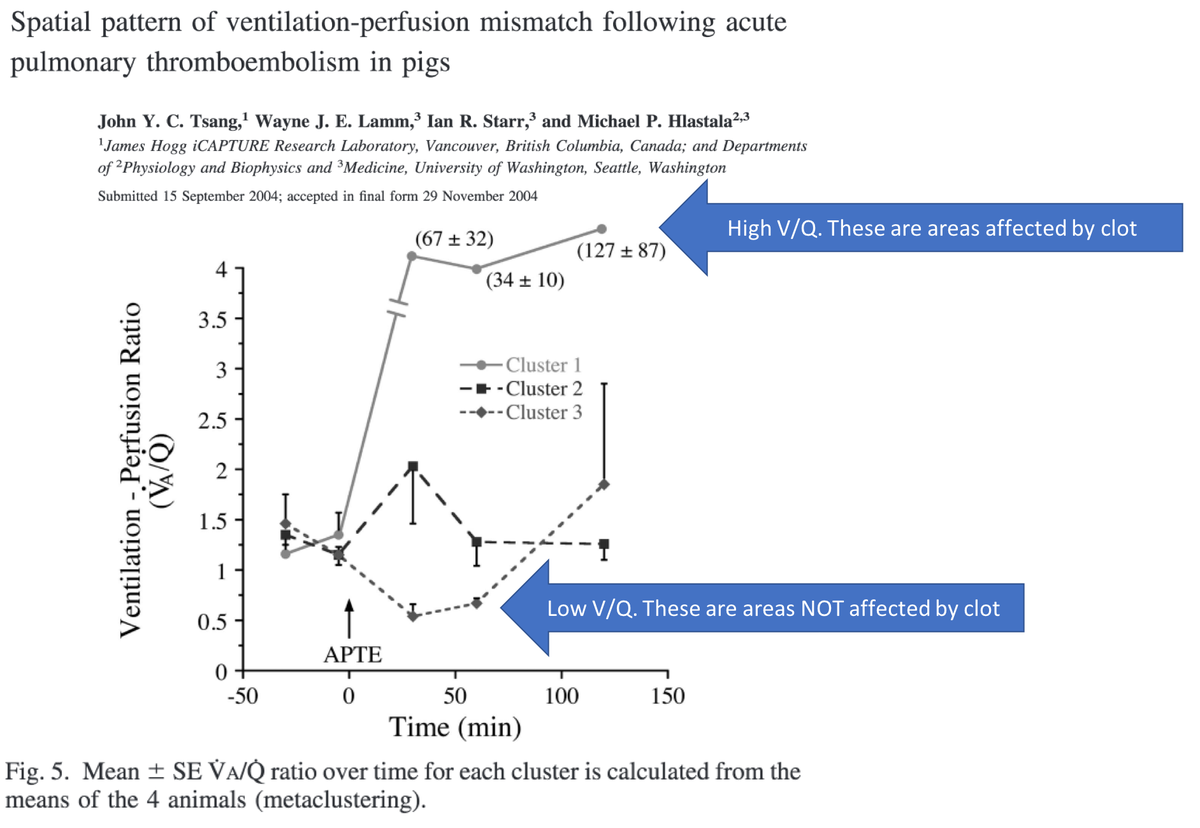
What causes this? In short, the blood that is "blocked" by the embolus is diverted to other areas of the lung. This:
*increases Q to those areas, with
*no matching change in V to those areas
Result: ⬇️V/Q ratio (by virtue of ⬆️Q)!
And: hypoxia!
ncbi.nlm.nih.gov/pubmed/9843561
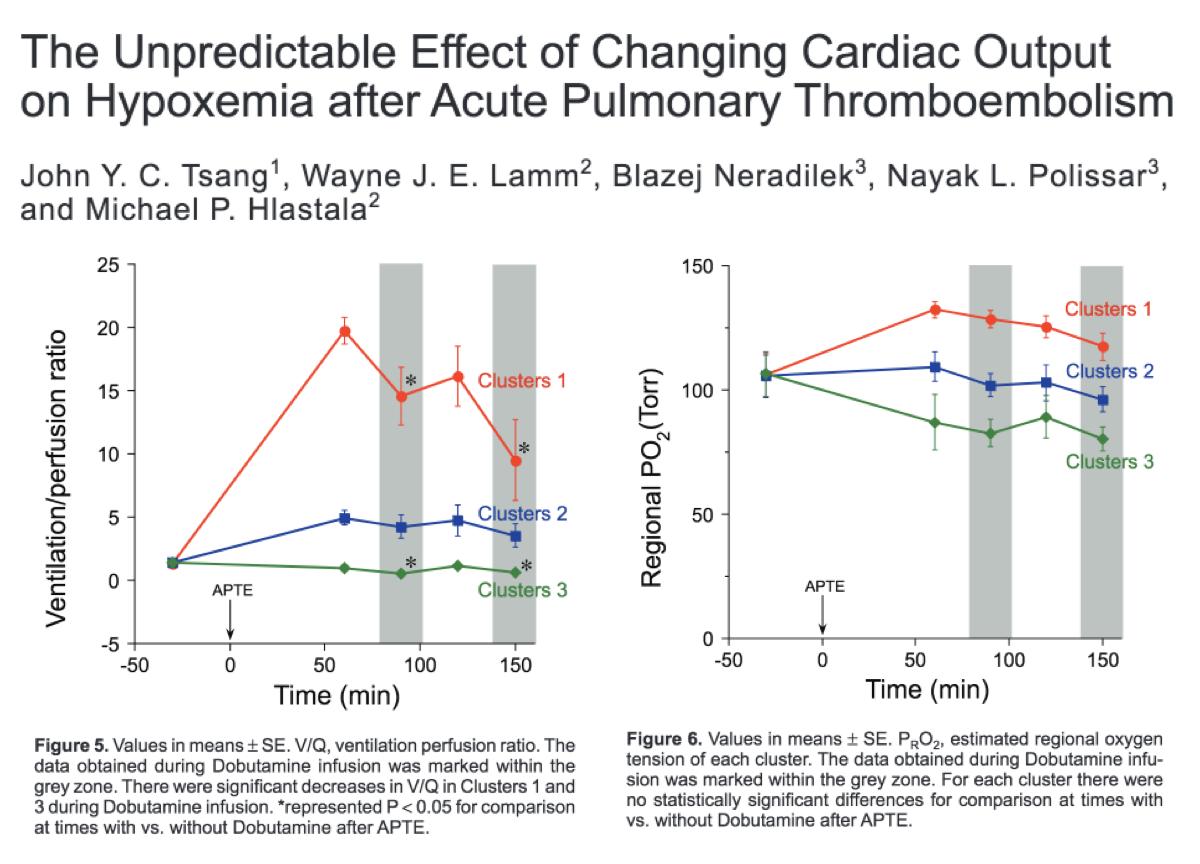
Using this explanation, what would you predict would happen if one used dobutamine to increased cardiac output in someone with acute PE?
At least one experiment suggests that V/Q decreases with an increase in cardiac output! The increase in Q was not offset by an increase in ventilation.
There was no consistent effect on PaO2 in this study, despite the decreased V/Q.
journals.sagepub.com/doi/abs/10.413…
The "diverted blood" theory of hypoxemia might also explain why some patients with massive PE and shock don't have hypoxia (see tweet 5).
If the blood hasn't diverted, it:
*doesn't contribute to systemic perfusion ➡ shock
*doesn't cause increased Q ➡ normal PaO2
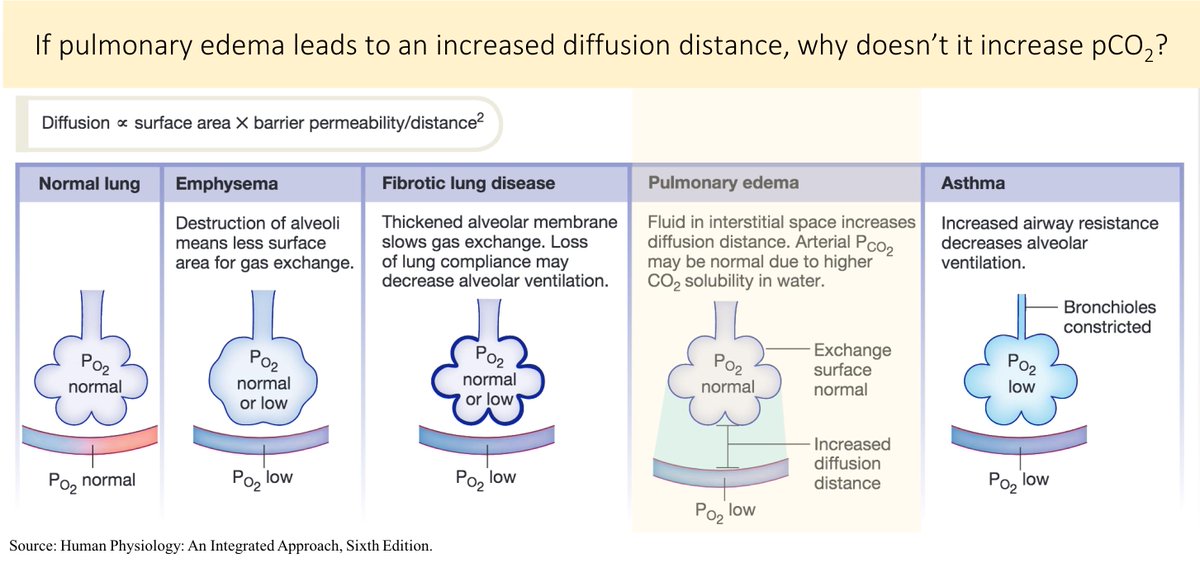
There are certainly other possible mechanisms for hypoxia in acute PE. Things like:
*atelectasis
*pulmonary edema
*bronchospasm
*shunt (e.g., via a PFO)
These may contribute, but don't seem to be the primary cause.
Let's return to one of the questions posed above.
Acute PE leads to hypoxia primarily via V/Q mismatch. But, what's altered? And, in what direction?
[V=ventilation; Q=perfusion]
Summary. In acute PE,
*blood that would otherwise perfuse the area of clot is diverted;
*this creates an increase in Q without a matching increase in V;
*this leads to a decreased V/Q ratio;
*resulting in hypoxia
If you found this thread interesting/useful, here is a link to others that attempt to answer pathophysiology mysteries/questions.
Thanks to @DavidJuurlink for pointing out an issue in the first tweet. The blood upstream of the clot hasn't yet been oxygenated (it's in the pulmonary arteries!).
But, it's "blocked" by clot. So, the question remains: how would it contribute to hypoxia?
In order for this blood to contribute to hypoxia, it could be shunted to the arterial circulation. This has been suggested by some on this thread (eg @strain_rate).
The studies I cite above support the major mechanism being diversion of blood, leading to increase in Q.