Why is "Routine Echocardiography in Hemodynamically Stable Patients with Acute Pulmonary Embolism" a #TWDFNR?
This question was addressed in this month's @JHospMedicine by @PaulBerglMD et al.
Here's a thread to complement their awesome review.
journalofhospitalmedicine.com/jhospmed/artic…
Let's start with a case and question. The case is taken from the review by @PaulBerglMD et al. Review it and answer the question in tweet 3.
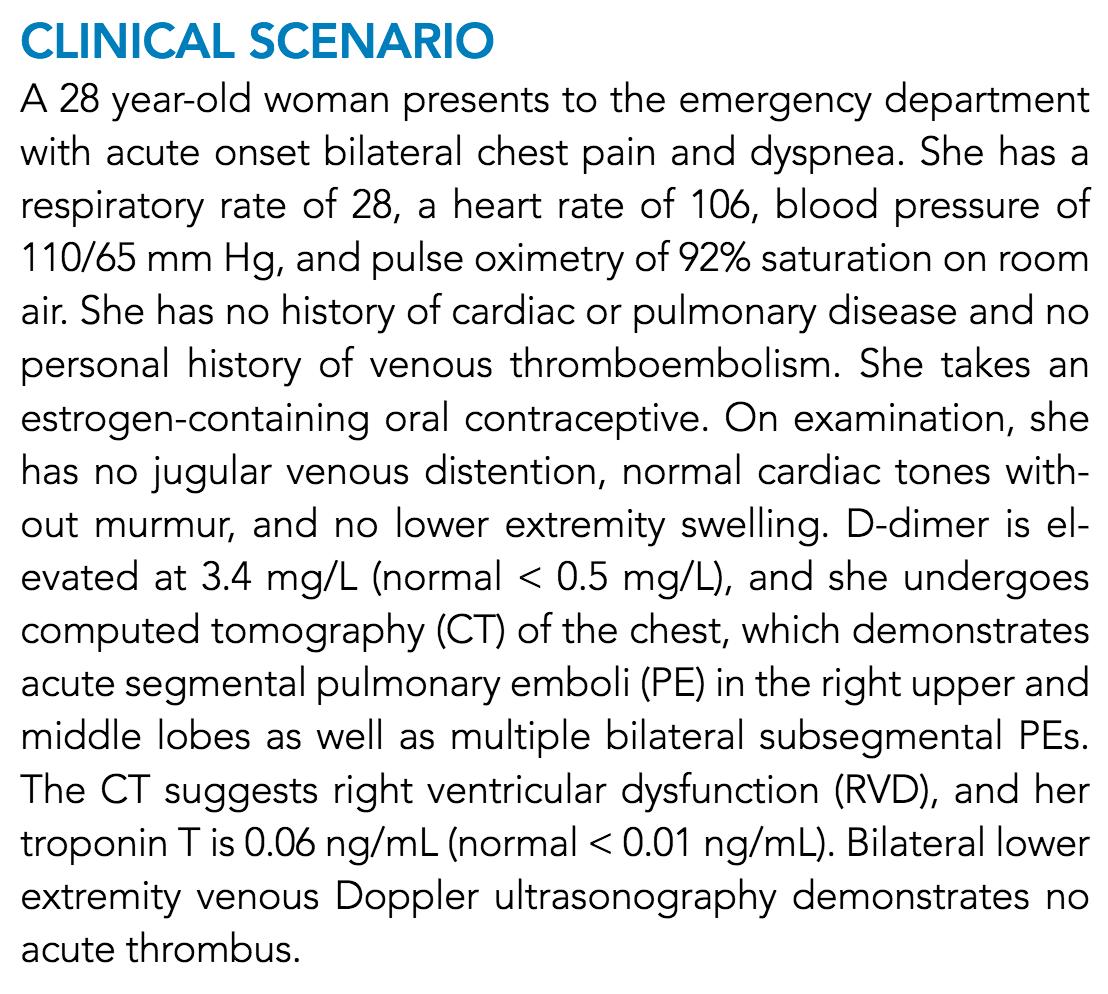
Would you order suggest that this patient with stable pulmonary embolism (PE) undergo echocardiography (echo)?
If you answered "yes", your aim may be to further risk stratify this patient.
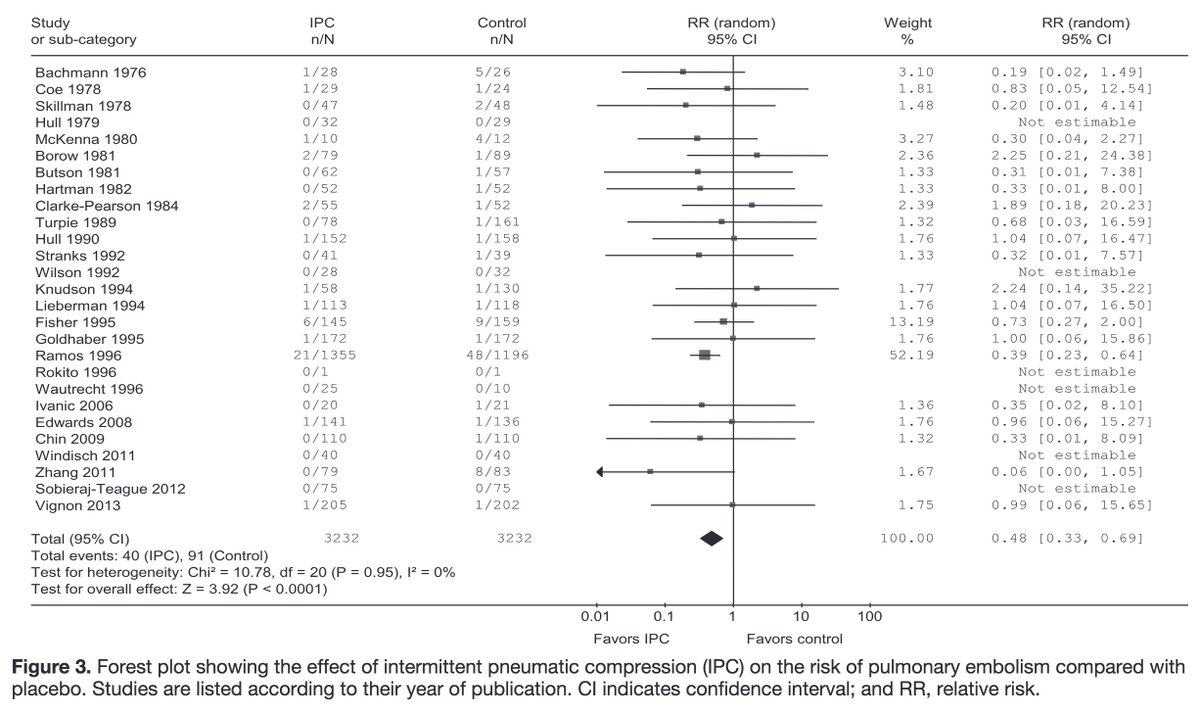
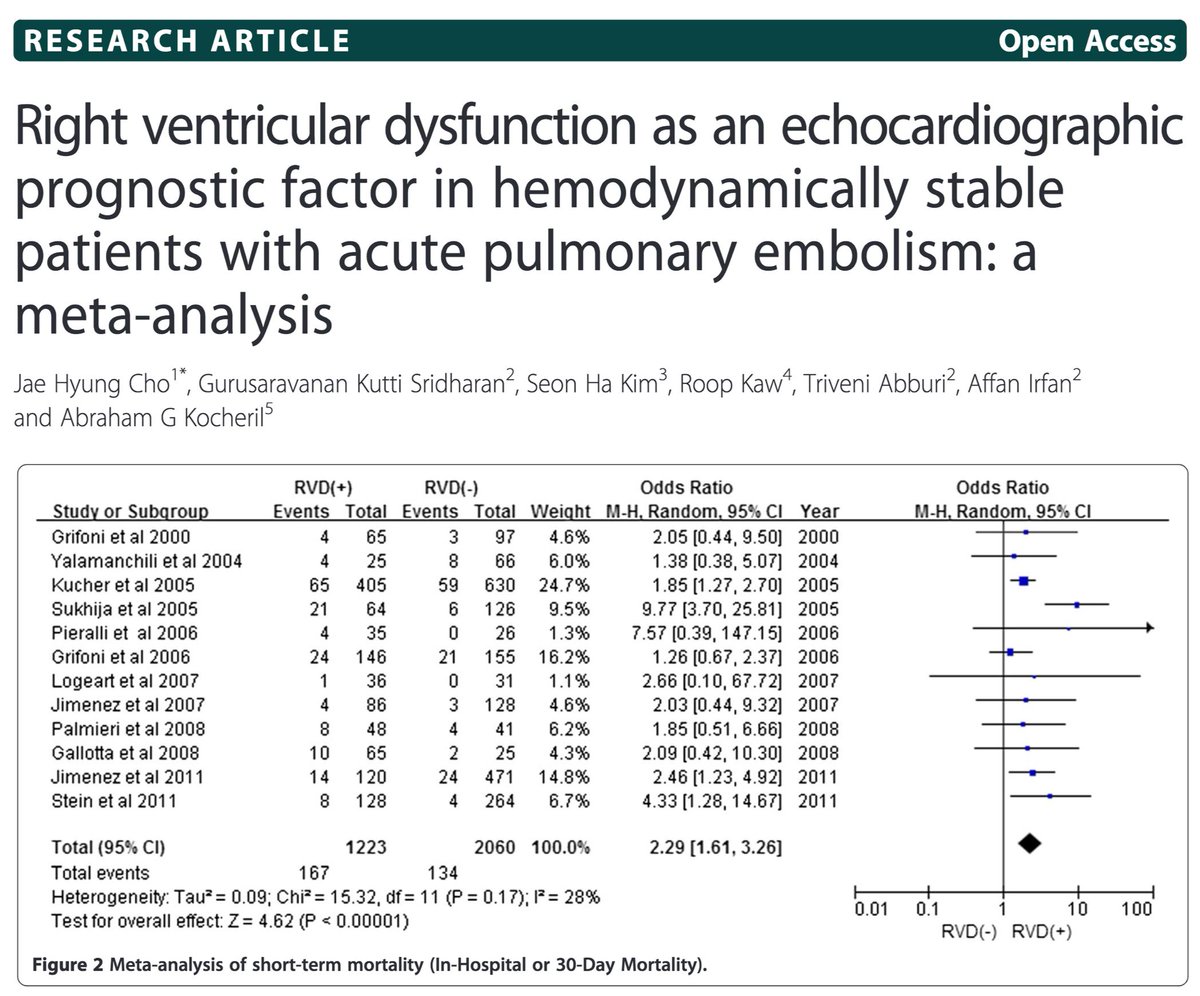
Some data supports this. One meta-analysis found an OR of 2.29 for short term death in patients with stable PE found to have right ventricular dysfunction (RVD) on echo.
ncbi.nlm.nih.gov/pubmed/24884693
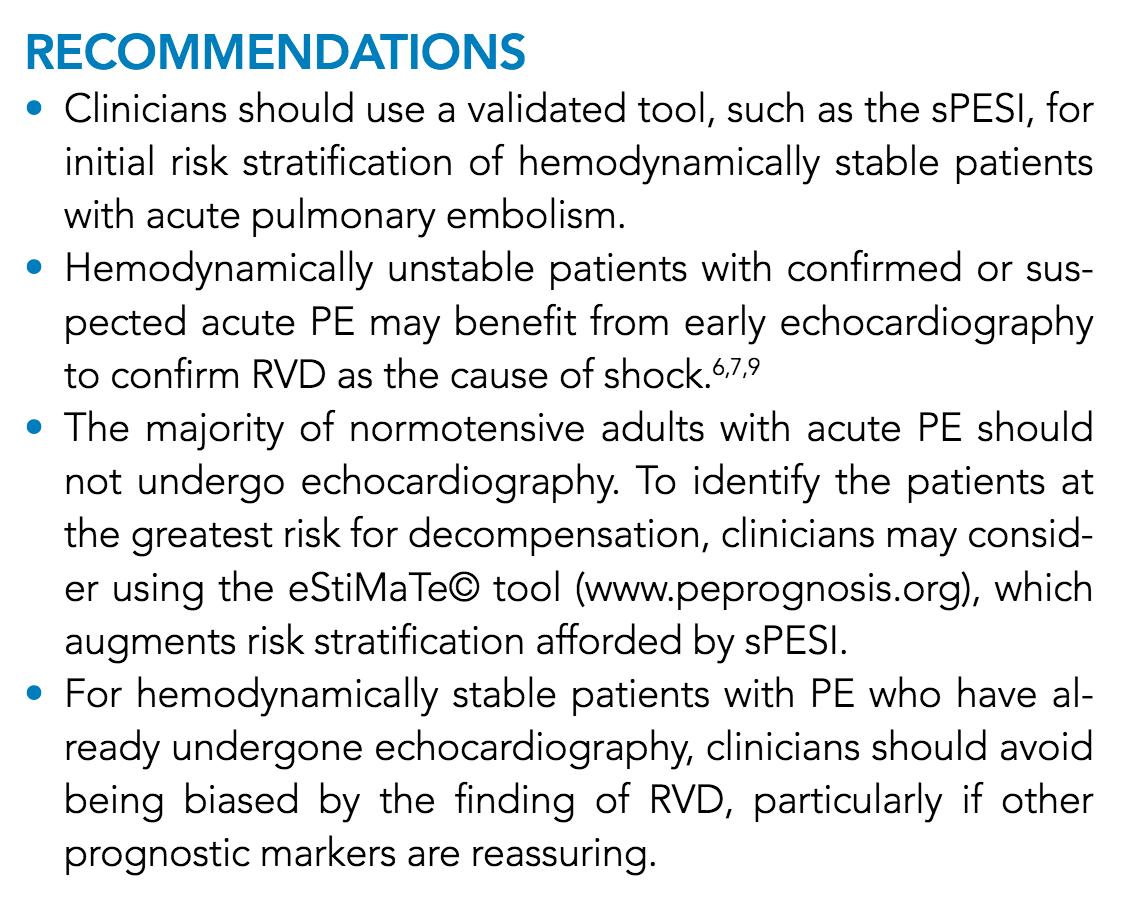
The authors of the @JHospMedicine review identify four reasons why echo for stable PE is a #TWDFNR:
(1) phenotypic expression of RVD varies widely
(2) even with RVD, the adverse event rate is low
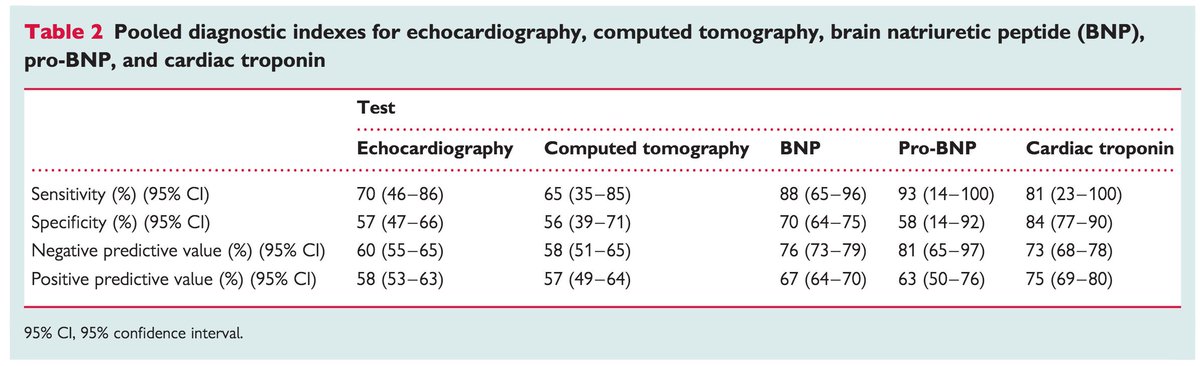
(3) RVD on echo adds little over biomarkers
(4) harm may result
For this thread, we'll cover the third argument.
The review is #openaccess and can be read for those who want to read all the arguments presented by @PaulBerglMD et al.
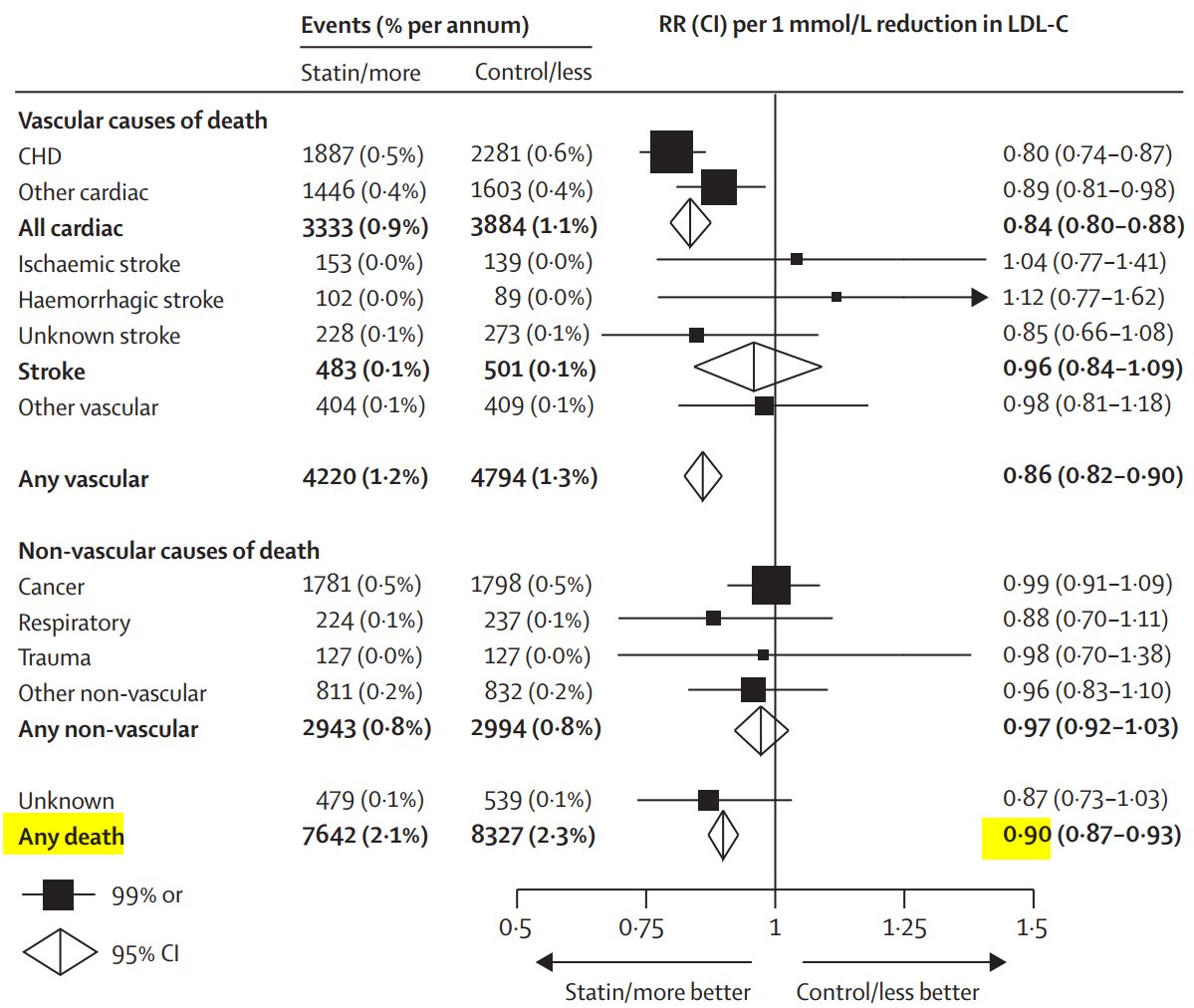
Regarding "RVD vs. biomarkers", one meta-analysis found the following unadjusted ORs for short-term death:
RVD = 2.4
BNP = 9.5*
Troponin = 8.3*
[*the cutoffs varied based on the study]
This suggests that RVD may add little once one has BNP/troponin.
ncbi.nlm.nih.gov/pubmed/18495689
Instead of routinely using echo in stable PE, the authors suggest using validated risk stratification models including the simplified PESI (sPESI) and the eStiMaTe© calculator.
These provide estimates for 30-day mortality.
mdcalc.com/simplified-pes…
riete.org/estimate/
Here are the final set of recommendations offered by @PaulBerglMD, Adrian Umpierrez de Reguero, and Jayshil J Patel.
For the patient in tweet 2, the sPESI and eStiMaTe© predict 30-day mortality rates of 1.1% and 0.4%. Assessing for RVD on echo would not add value.
If you're interested in reading more about why routine echocardiography in hemodynamically stable patients with PE is a #TWDFNR download the open access article at @JHospMedicine
journalofhospitalmedicine.com/jhospmed/artic…