It’s time for a #tweetorial on hypersensitivity pneumonitis. It’s a greatly misunderstood entity. Potentially treatable, so can be very good news. OTOH, misdiagnosing UIP as chronic hypersensitivity pneumonitis can be very bad.
Follow this thread for a #pathtweetorial
Let’s start with a poll regarding a common misconception. What is the predominant inflammatory cell in hypersensitivity pneumonitis?
Hypersensitivity pneumonitis is an inflammatory reaction that occurs in individuals (classically never-smokers) who are exquisitely sensitive to an organic antigen.
Obvious exposures (moldy hay=farmer’s lung) can be fairly straightforward to recognize clinically.
Let’s recap:
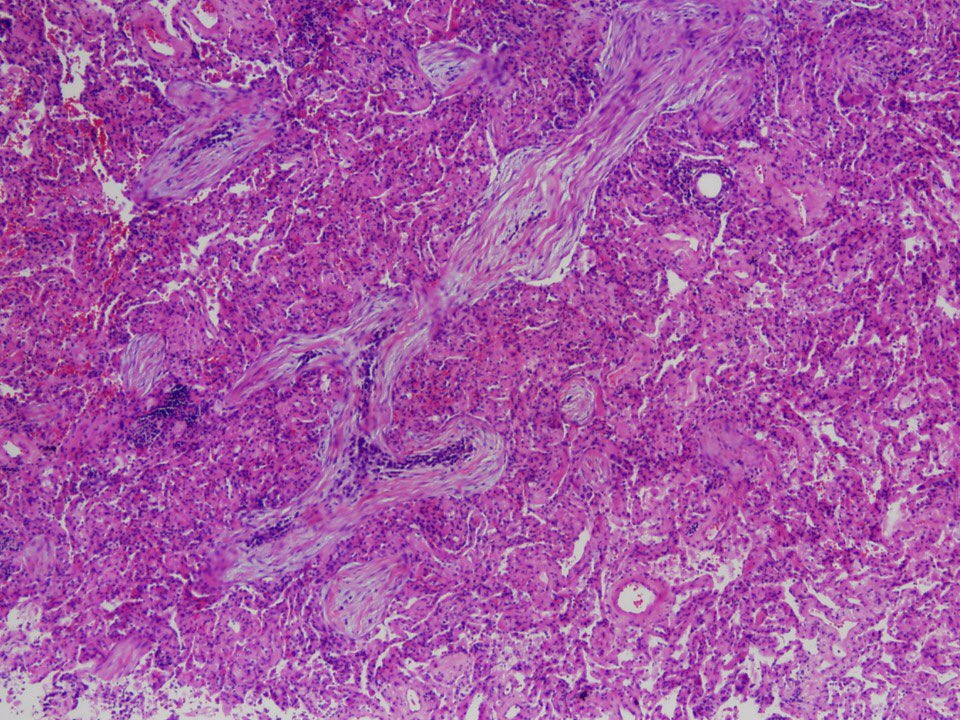
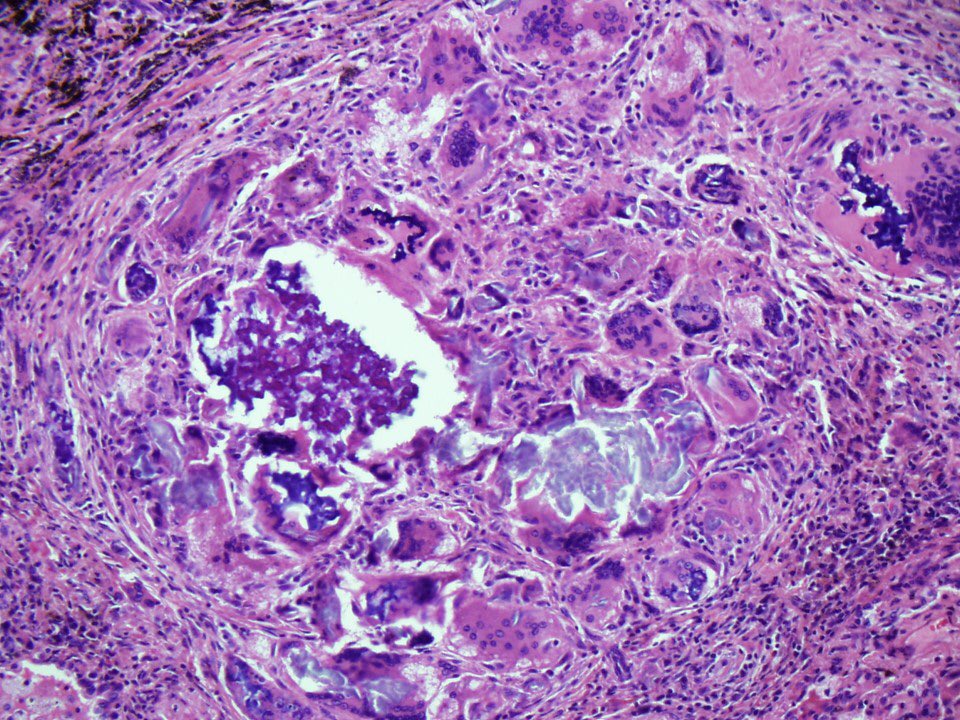
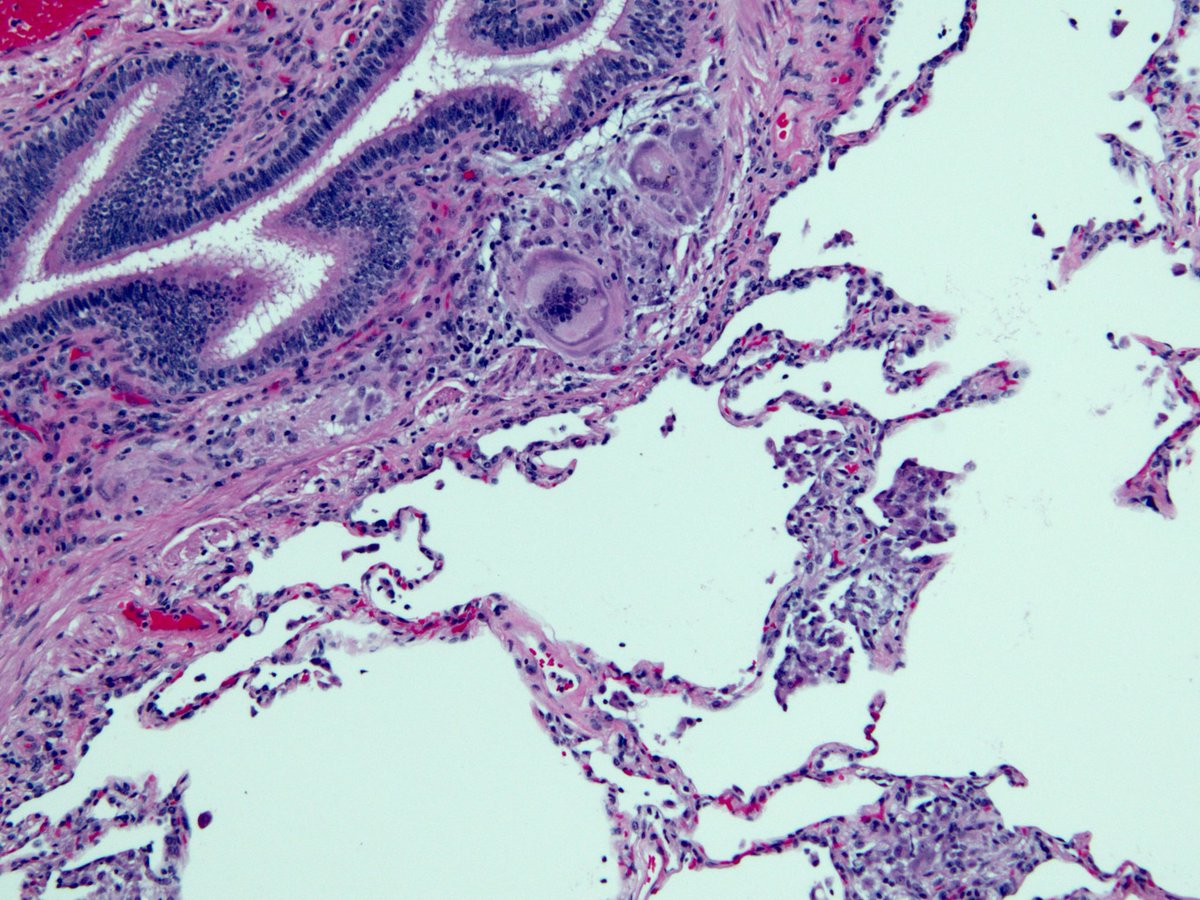
Chronic bronchiolitis + interstitial lymphocyte infiltrate + occasional giant cells.
Read more about the #pathology of this disease here:
emedicine.medscape.com/article/207843…
If you want to see a video with a detailed discussion of the pathologic findings in hypersensitivity pneumonitis, check out this YouTube video I made:
#pathology #pulmpath
Eosinophils are NOT a feature of hypersensitivity pneumonitis. Most cases don’t have ANY!
Lymphocytes ✅✅✅✅
Eosinophils ❌❌❌❌
In terms of the inflammatory response, hypersensitivity pneumonitis is more like TB (type 4) than asthma (type 1)
Let’s examine the imaging, since that’s the leg that clinicians rely so heavily on.
Remember, we are talking about “subacute” hypersensitivity pneumonitis, the least controversial form. Here an expert radiologist describes the “head cheese sign”
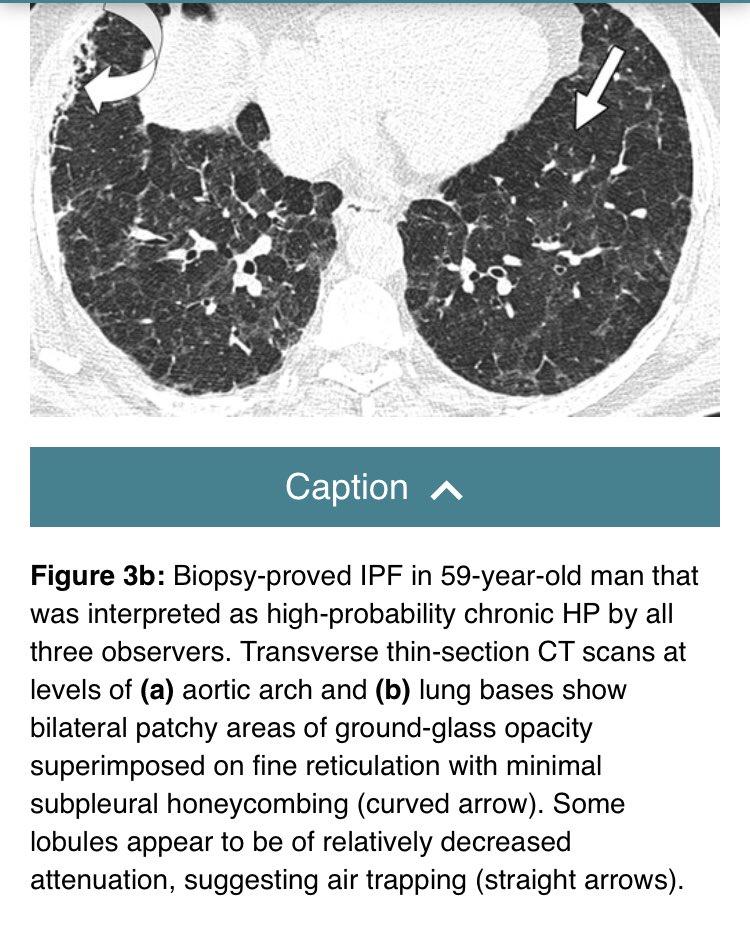
Agreement goes out the window when it comes to “chronic hypersensitivity pneumonitis”, an entity in which fibrosis allegedly develops and progresses to an appearance very similar to UIP/IPF. Most of these cases behave very badly (like UIP).
So what makes them HP? Read on..
Often, this diagnosis is based heavily on “air trapping” on HRCT. This is truly a one legged table, resting solely on imaging. Can air trapping occur in UIP/IPF?
Answer: Yes!
This study by Sverzellati et al is a must-read:
pubs.rsna.org/doi/full/10.11…
If it walks like a 🦆 and quacks like a 🦆 it’s a 🦆, right?
The chronic HP camp says no. It looks like UIP and behaves like UIP. No exposure. Smokers. Elderly men. But air trapping makes it HP.
I don’t buy this argument. I think most of these are UIP/IPF.
I’m willing to buy chronic HP if the patient is a bird fancier and/or pathology is classic for HP in non fibrotic areas of the lung
But UIP doesn’t become HP just because of:
🔴 a few granulomas
🔴 chronic inflammation
🔴 “airway centered fibrosis”
🔴 air trapping
Optimal Rx of hypersensitivity pneumonitis: identify the source of exposure and get the patient away from it.
The next time you see a dyspneic never smoker with bilateral GGO and the head cheese sign on HRCT, ask them if they have pet birds.
🔴 End of #Tweetorial 🔴