Why is the acute treatment of "hypertensive urgency" a #TWDFNR?
This #tweetorial is meant to complement the recent publication: "Acute Treatment of Hypertensive Urgency" in @JHospMedicine
journalofhospitalmedicine.com/jhospmed/artic…
Case: A 71M with a history of HTN is hospitalized for cellulitis. On hospital day 2, the nurse pages you:
"Pt X with BP ____. Please advise". He has no symptoms or signs of end-organ damage.
What would be your threshold SBP to write for an as-needed anti-hypertensive?
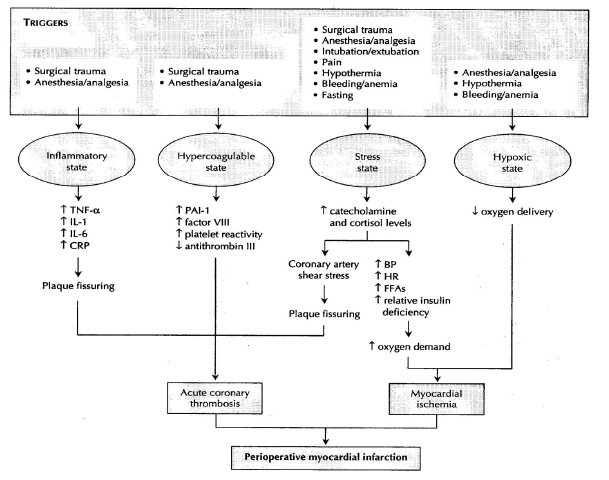
The treatment of hypertensive urgency is based on an assumption: if we do not lower the blood pressure now, something bad (e.g. stroke, MI, aortic dissection) will occur in the next few hours.
We aren't giving IV hydralazine to prevent a stroke two years from now...
To see why the treatment of hypertensive urgency is a #TWDFNR, it helps to review:
*evidence base
*pathophysiology
Much of the evidence base is drawn from outpatient and ED studies.
One of the studies covered in the new #TWDFNR review was by Patel et al, published in 2016 in @JAMAInternalMed. It included 58,836 outpatients with hypertensive urgency.
426 (0.72%) were sent to the hospital
100 (0.17%) were admitted
ncbi.nlm.nih.gov/pubmed/27294333
This study informs one key principle: in those who have no evidence of end-organ damage the benefits of blood pressure lowering accumulate over months to years, not hours.
As the authors of the #TWDFNR review note, "the human body has adapted to withstand wide variations in blood pressure." For example, autoregulation protects the brain highs and lows in systemic BP.
But, these the autoregulatory range appears to shift in those with HTN.
This was demonstrated in a series of studies in the 1970s.
You'll notice in the picture that as one drops from a MAP of 150 (eg 215/118) to a MAP of 110 (eg 160/85) that some curves suggest decreased cerebral perfusion. This is a 25% decrease in SBP.
ncbi.nlm.nih.gov/pubmed/4692673
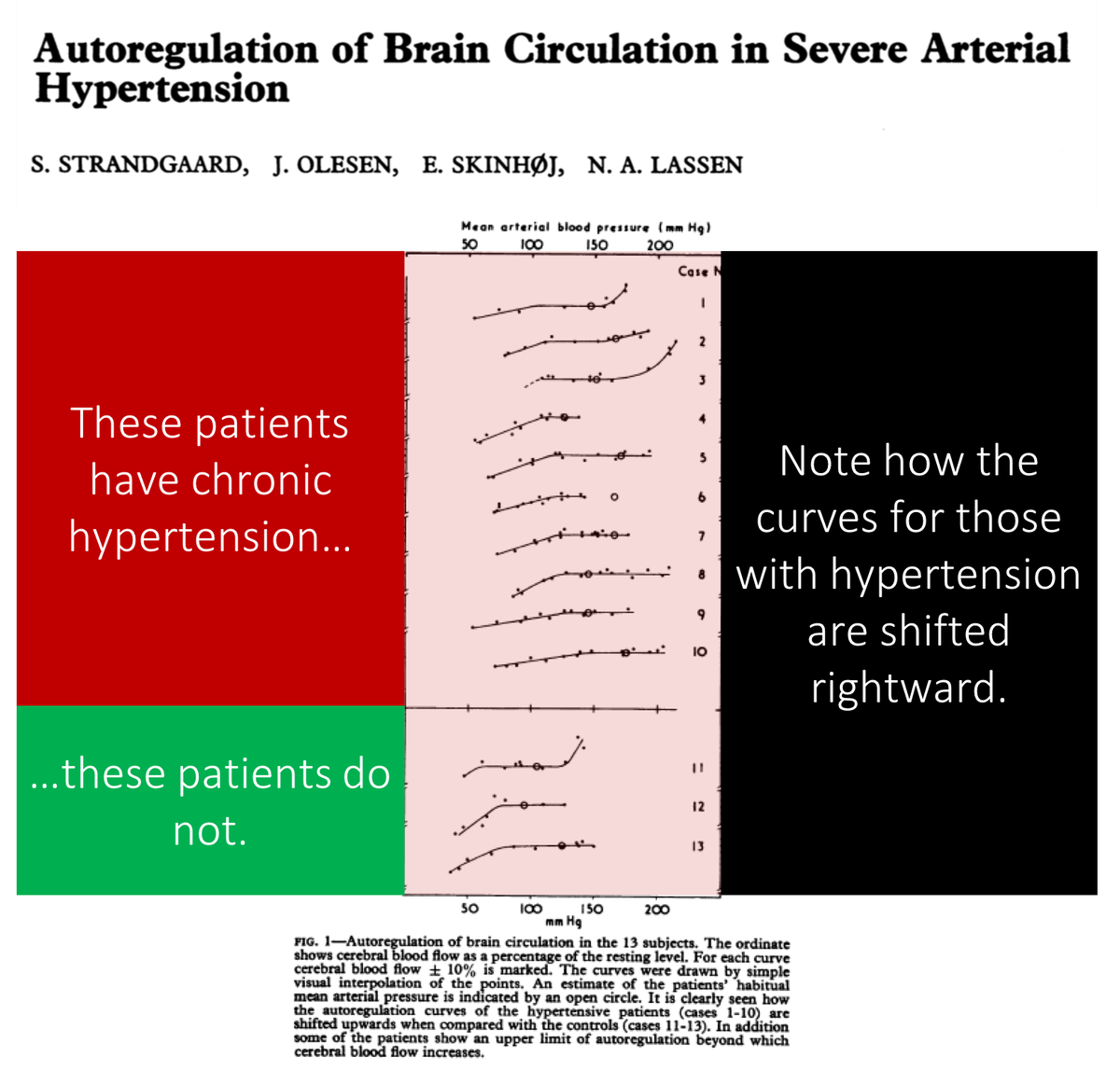
Even with a drop of 25% in SBP (the upper limit of what is deemed appropriate), cerebral perfusion may decrease enough to cause lightheadedness, falls, and even strokes.
This has been seen with myriad quick-onset anti-hypertensives, as noted in the review.
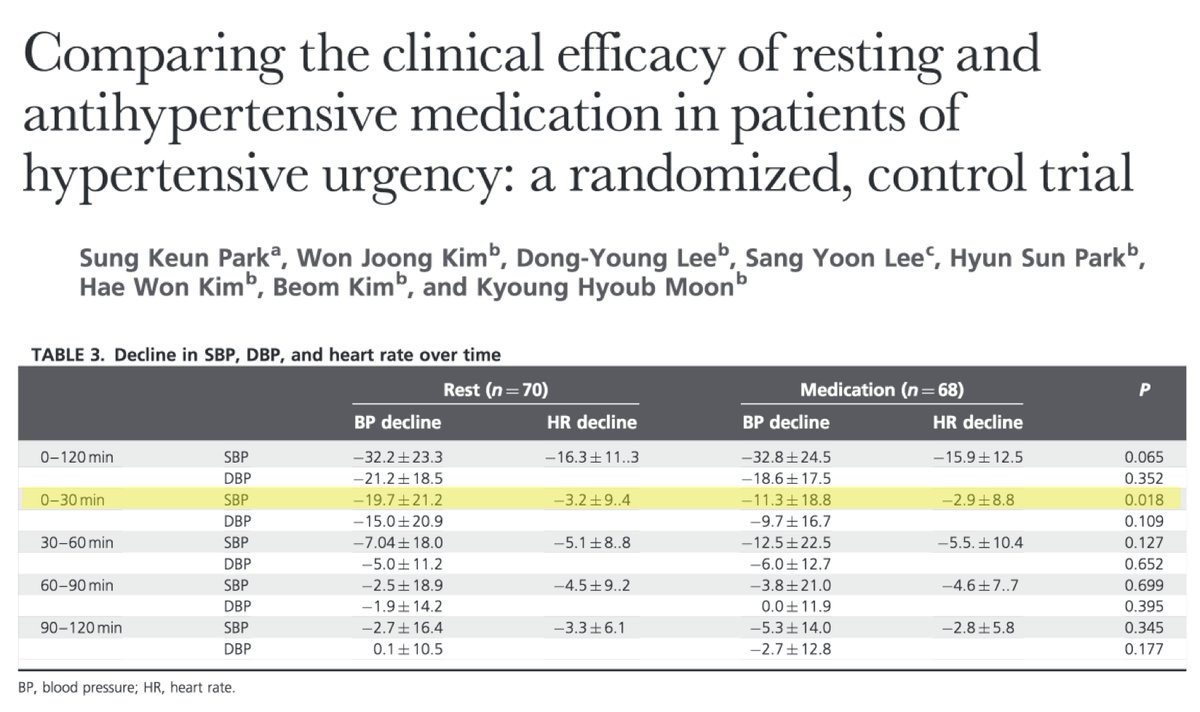
It also turns out that rest is quite an effective treatment for hypertensive urgency. This should come as no surprise given the trends in blood pressure we all observe in our patients over a 24-hour period.
One of the studies reviewed actually found that telsimartan was equally effective at blood pressure lowering at 2 hours and MORE effective at 30 minutes.
ncbi.nlm.nih.gov/pubmed/28244897
What do you think? What would be your SBP threshold now?
If you find any of the above interesting or want to get a fuller picture of the argument, consider reading the full review published this month in @JHospMedicine
journalofhospitalmedicine.com/jhospmed/artic…
The original tweet doesn’t make clear that REST was as effective as telmisartan at 2 hours and more effective at 30 minutes.