⚡️Is Urea a good solute to assess Adequacy ?
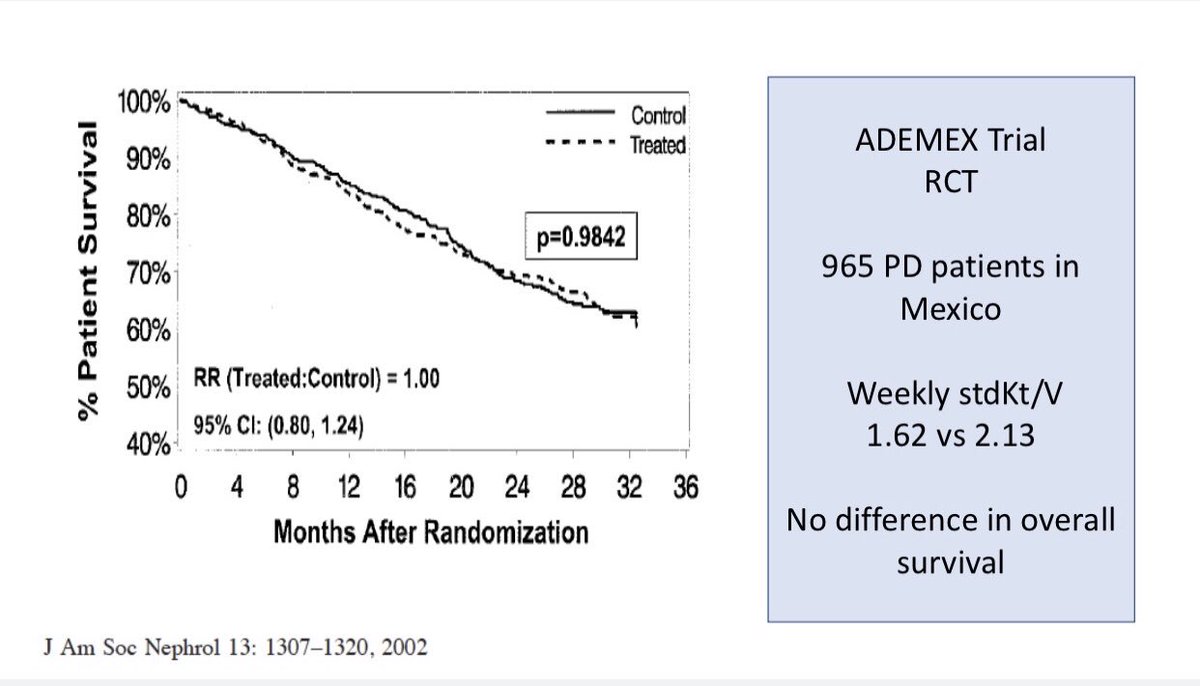
⚡️Is Kt/V urea a good Adequacy test?
⚡️Should ‘time on dialysis’ be an independent measure of Adequacy?
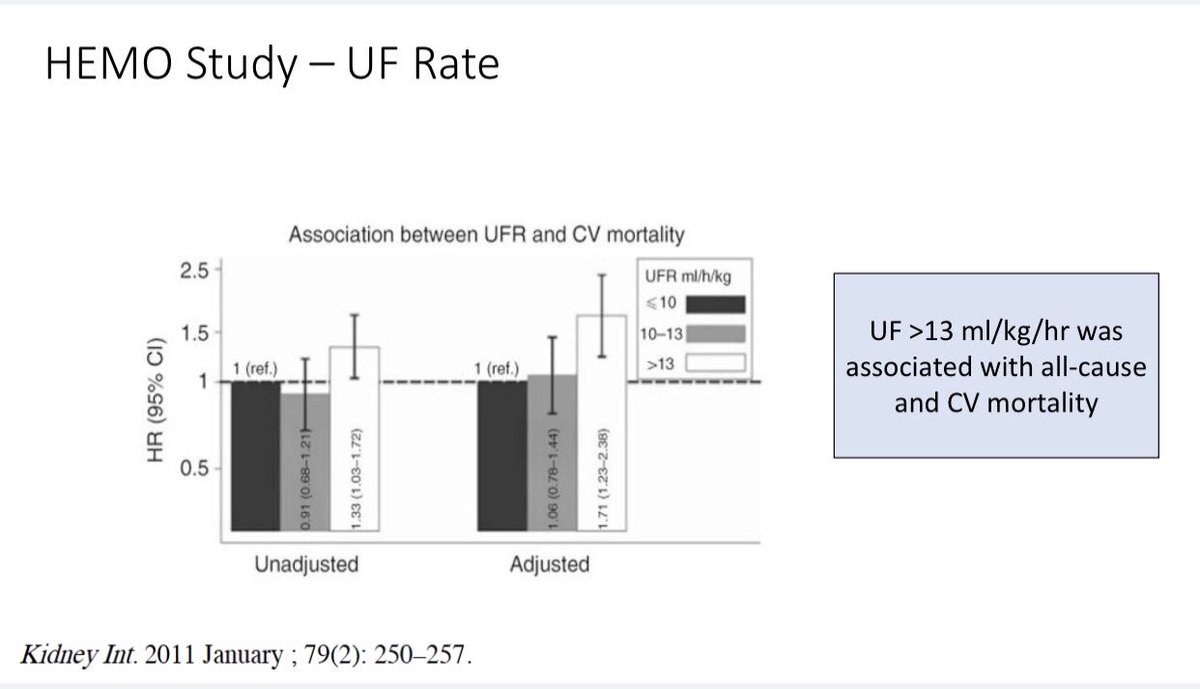
⚡️Should ‘UF rate’ be a measure of Adequacy?
@RenalFellowNtwk
#NephPearls
⚡️Total solute removal
⚡️Rate of fluid removal
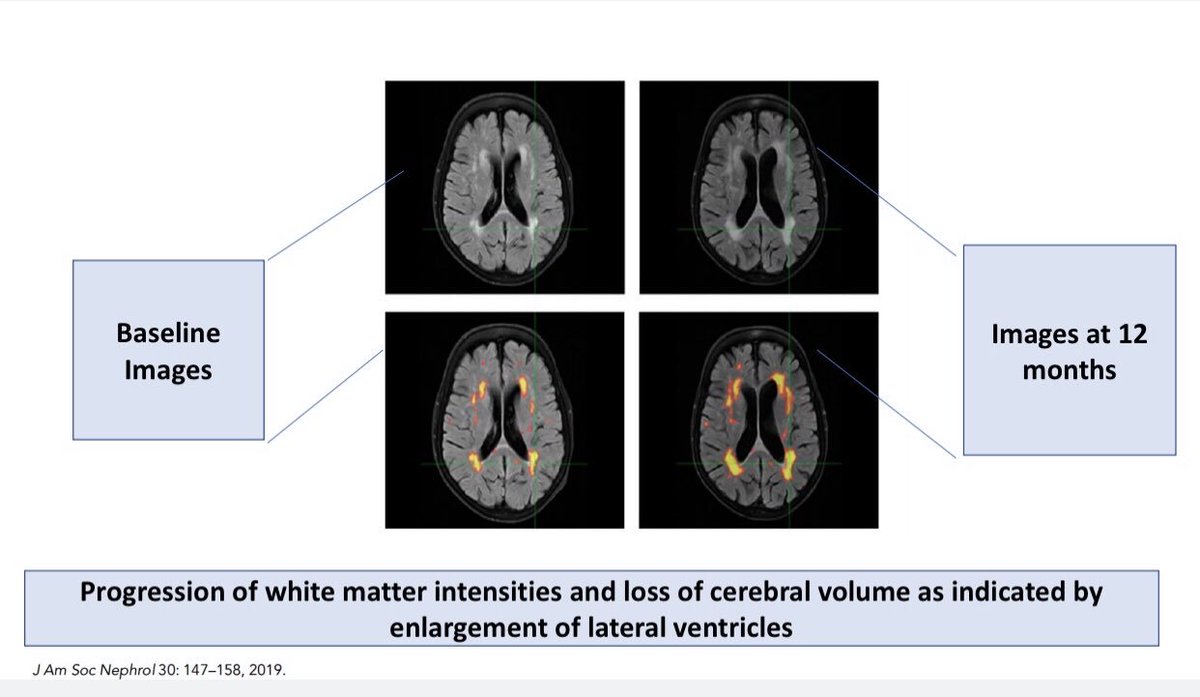
⚡️Middle Molecule Clearance
⚡️Phosphorus removal
⚡️Yes
-KDOQI recommends a minimum of 3hrs/session for 3x/wk HD
-European Practice Guidelines recommends at least 4 hrs HD/session
-Of course, one has to consider the RRF
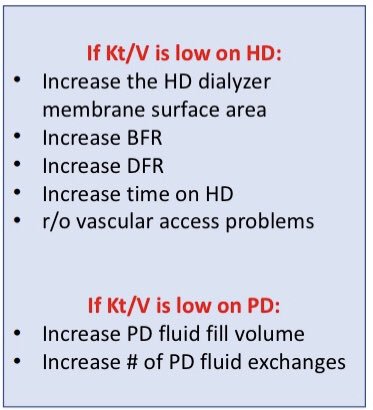
⚡️Target minimum spKt/V urea > 1.2 and target 1.4 or > for 3x/week HD
⚡️Target weekly Kt/V of > 1.7 for PD
⚡️Target Kt/V for FHD is opinion-based to meet the weekly standard
Kt/V of 2.0