VENOUS STASIS LEG ULCERS!!!
A #tweetorial for the #dermtwitter, #medtwitter, #medstudenttwitter, and #hospitalist crowd. 📸:@dermnetnz #medthread
Let's start with a question - What percentage of leg ulcers do you think is caused by venous stasis?
How do you differentiate from other ulcer types? Pts with stasis ulcers have had venous insufficiency for some time. For that reason, the rest of the leg is going to show those changes:
- bilateral brawny skin discoloration
- leg edema
pc: wikem.org/wiki/Venous_st…

In addition to venous insufficiency, these patients can get stasis dermatitis that can look like eczema (pic 1), or just like acutely swollen red tender legs (pic 2)!
As @MishaRosenbach would say, "bilateral cellulitis is case reportable," so if you see that, think stasis!


A quick reminder that this type of eczematous eruption in skin of color may look different! Redness/erythema is a lot harder to see (see photo)! So just because you don't see the redness doesn't mean it's not inflamed!
pc: medicalnewstoday.com/articles/32506…

There are of course risk factors for venous stasis, which are mainly things that cause venous congestion, like:
✅history of DVT
✅varicose veins
✅h/o multiple pregnancies
✅cardiac and liver disease
✅older age
✅obesity
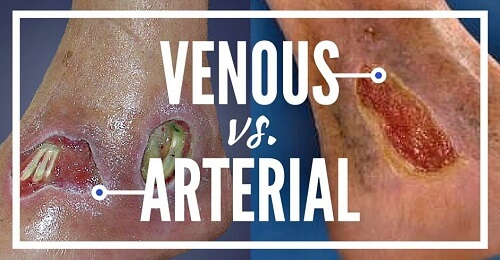
What about your ddx?
Arterial ulcers are on the ddx, but they are usually more "punched out," and in a pt with a h/o claudication & hairless/shiny legs). I remember being taught in med school to think of blood as soil that needed to grow hair!
pc: blog.wcei.net/2014/12/venous…
There are many other possible causes for leg ulcers, so always feel free to call your friendly neighborhood #dermatologist or @DermHospitalist for help. Sometimes a biopsy may help, but often, a good clinical exam is enough for us to make the diagnosis & help with treatment!
So how do we treat?
1⃣ Make sure there's no infx. We may tx with topical or systemic abx, depending on the exam. I don't use superficial wound swabs much, as I think of that as just catching colonizers.
NB: Given its propensity to cause a contact allergy, avoid triple abxs!
2⃣Clean up the ulcer. We do this with enzymatic debridement (eg: collagenase) or mechanically at the bedside (which we'll do), or in the OR (w/ surgery).
3⃣ Huge ulcers probably will get a wound vac, or a graft in some circumstances. Smaller ones can be healed secondarily.
4⃣ For dressings, I like to use a nonstick one & covered with gauze. From a #derm perspective, we don't like it to dry up (keep it moist!)
Wet->dry dressings are painful, & I almost never use them! They're good to debride, but I think there are nicer ways to do it.
5⃣ And perhaps most important: COMPRESSION! These pts need to tx the underlying cause of venous stasis, so pushing the blood up w/ tights is necessary to tx AND prevent ulcers.
Standard issue TEDs aren't great. Pts should be measured for the right fit. I like 20-30 mmHg.
Recap -
✅Stasis ulcers are 2/2 bad venous congestion. Look for exam findings c/w that.
✅Remember your ddx to r/o other causes since tx changes!
✅ Tx infection 1st, then clean/debride & dressing changes.
✅Compression to prevent future ulcers!
✅ #Derm is here to help!