#AmazingGrady, Day 5
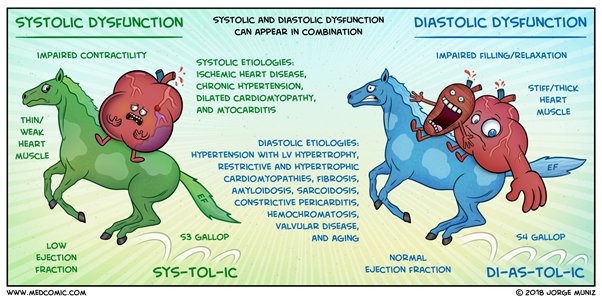
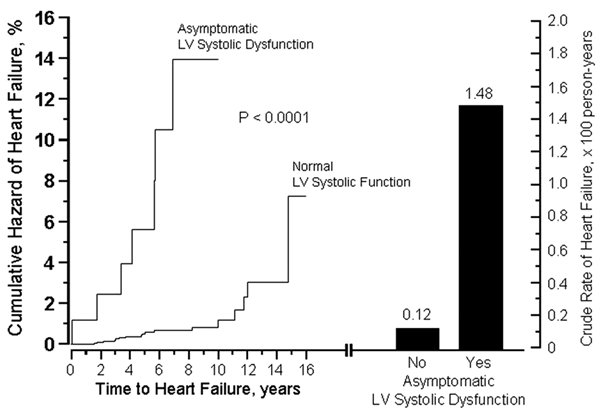
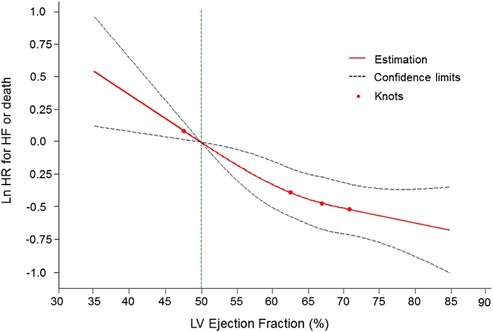
I was presented a patient with structural heart disease. Nonischemic HFpEF, to be exact.
PND. Orthopnea. S3 on exam. Reported some intermittent palpitations but EKG NSR, some LVH w/strain.
Admitting diagnosis: Acute decompensated HF
So far, so good.

Work rounds the next day:
Diuresis is going well. Responding to loop diuretics. And shout out to hydralazine for the double whammy of BP control + afterload reduction.
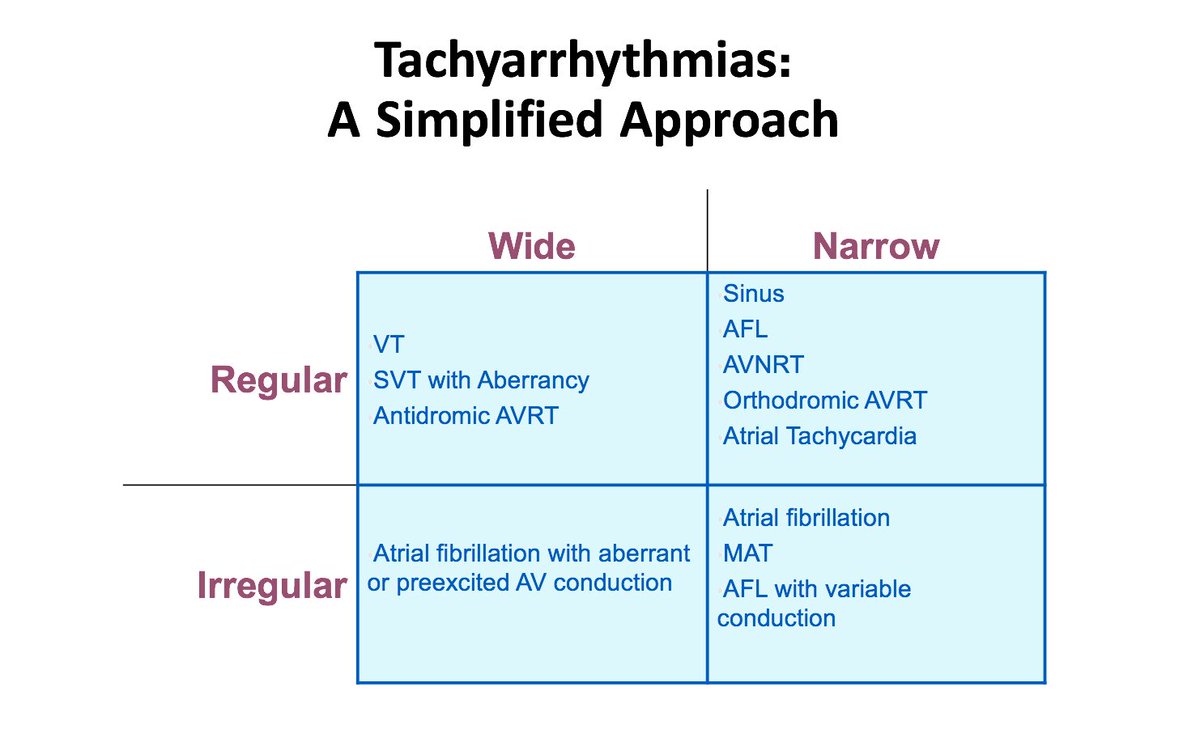
“Oh. But she had palpitations again. And on tele she was in atrial fibrillation.”
Hmm. Ok.
The atrial fibrillation came in paroxysms at first but then decided to stick around for a while. Still hemodynamically stable. We focused on rate control mostly. We started anticoagulation.
And kept on with diuresis.
Cool? Cool.
Next day:
S: Urinating a lot. Brief episode of CP overnight—negative ACS workup.
O: In and out of AF overnight. In AF now. HD stable. Can’t hear S3. Crackles at bases. Warm.
A: 1.ADHF 2. AFib w/RVR
P: Diuresis, afterload reduction, rate control . . . .
Cards following.
Scrolling labs.
Wait. What?
TSH—nearly undetectable.
Wait. What?
Me: “Have you ever been told that you have an overactive thyroid?”
Her: “A overactive who?”
Launch into a spiel on ⬆️T4. She assures us that all of this is new to her. And this patient would’ve known.
Shoot. Shoot. Shoot.
1. She had structural heart disease.
2. She had acute decompensated heart failure.
3. She took her meds and adhered to her diet.
4. She had a new diagnosis of atrial fibrillation.
For #4, though? I hadn't really thought too hard about why beyond #1.
I anchored. I didn’t think beyond the structural heart disease as the cause of the AFib. Nor did I give her credit for tight adherence.
Anchoring bias.
And some regular bias, too.
Honestly? I’m not fully sure who even ordered the TSH. But I’m glad they did.
Okay, so check it:
I’m not a self-deprecating type. I just want to learn from what happens around me, get the lesson, and model accountability. My quick close on the AFib blinded the whole team from looking at other causes.
Such as hyperthyroidism. Hello?
Hyper-doggone-thyroidism. A treatable, reversible cause of AFib, man! Which yes, she was entitled to have.
Dang it!
We debriefed on it as a team. (And yeah, debriefing is good for coulda-woulda-shouldas that don’t turn out super awful, too.)
My debrief:
Last patient on rounds that day.
A bread and butter admission.
With a bread and butter twist.
Except we overlooked a (reversible!) bread and butter etiology.
It was a fast-closer set up, man. With me at the wheel.
Here's my practice-based learning and how I plan to improve from this:
1. Take a step back and think.
2. Announce to the team when I feel like we could be in a system/anchoring/fast-closing land mine.
3. Take another step back and think.
4. Ask my team to think with me.
And lastly? Just keep trying, man. Trying to know better, do better, and be better.
Which includes reading/reinforcing knowledge to strengthen the lesson. Here’s the paper I read tonight on thyroid disease and the heart.
ahajournals.org/doi/10.1161/CI…
That's all. 🤓
#staywoke