How about a #Tweetorial on immunotherapy in quiz and answer form? Let’s try it! I’ll post a quiz in one tweet and then the answer in the next, and so on. Scroll down to follow the thread!
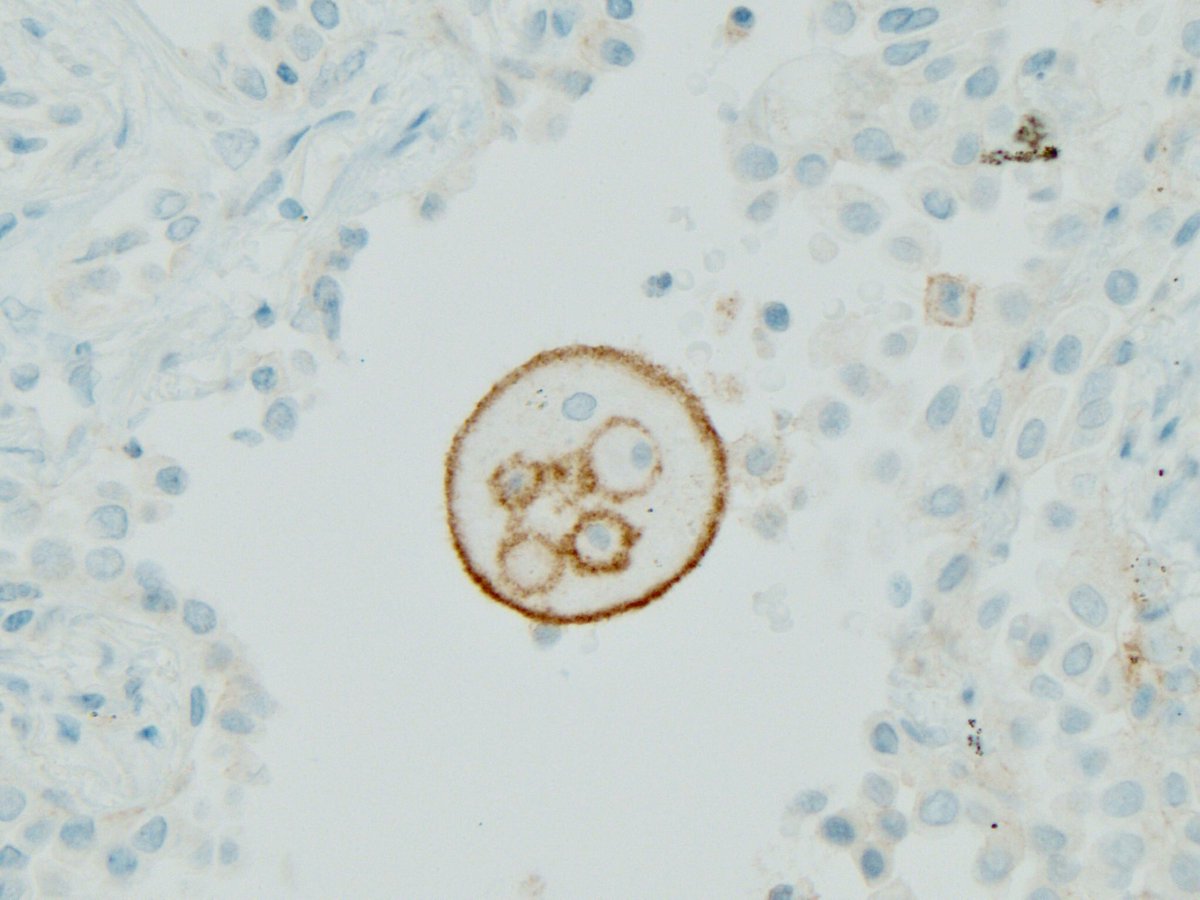
#pathology #pulmpath #ihcpath #pdl1 #Immunotherapy #pathtweetorial
First question. When PD-1 on T cells binds PD-L1 on tumor cells, what happens to the T cells?
The correct answer is that the binding of PD-1 to PD-L1 INHIBITS T cell killing of tumor cells.
See nice tweet on this by @kis_lorand
Q2. Anti PD-1 immunotherapy affects primarily which type of immune cells?
Test your knowledge by answering the quiz and then scroll to the next tweet for the correct answer!
Q3. James Allison won the 2018 Nobel Prize for the discovery of CTLA-4. Who won the Nobel along with him for the discovery of PD-1?
PD-L1 tests are often, but not always, required before immunotherapy is given. A diagnostic test that is mandatory before a certain therapy can be given is called:
The correct answer is “companion diagnostic”. These tests MUST be done before the drug is given, per the FDA.
Companion diagnostics are not just limited to immunotherapy. Herceptin and Gleevec require companion diagnostics.
ncbi.nlm.nih.gov/pmc/articles/P…
A “cousin” of PD-1 is CTLA-4. Like PD-1, it’s a “brake” on the immune system. And like inhibitors of PD-1 or PD-L1, turning off this brake is useful in cancer therapy. Which of these drugs is directed against CTLA-4?
Q6. When interpreting 22C3 PD-L1 immunohistochemistry for non-small cell lung carcinoma, which of these is true when calculating the TPS?
The answer is that you must evaluate tumor cells only for this assay and indication.
Immune cells are NOT counted (that’s SP142).
Any membrane staining of any intensity in tumor cells is counted.
The cutoff for “positive” depends on setting
Q7. A remarkable aspect of #immunotherapy is that DURABLE complete responses are possible even after DISCONTINUATION of the drug. With pembrolizumab for metastatic melanoma, what is the 24M survival reported in complete responders AFTER stopping Rx?
The correct answer is 89.9% (data from Keynote 001)
The theory is that unleashed T cells keep destroying tumor even after the drug that unleashed them is stopped
The hope is that some of these patients might be cured!
ascopubs.org/doi/10.1200/JC…
The correct answer is lupus-like arthritis. These mice also developed glomerulonephritis. Since PD-1 deficient nice were developing autoimmune diseases, this meant PD-1 was somehow keeping the immune system in check.
academic.oup.com/intimm/article…
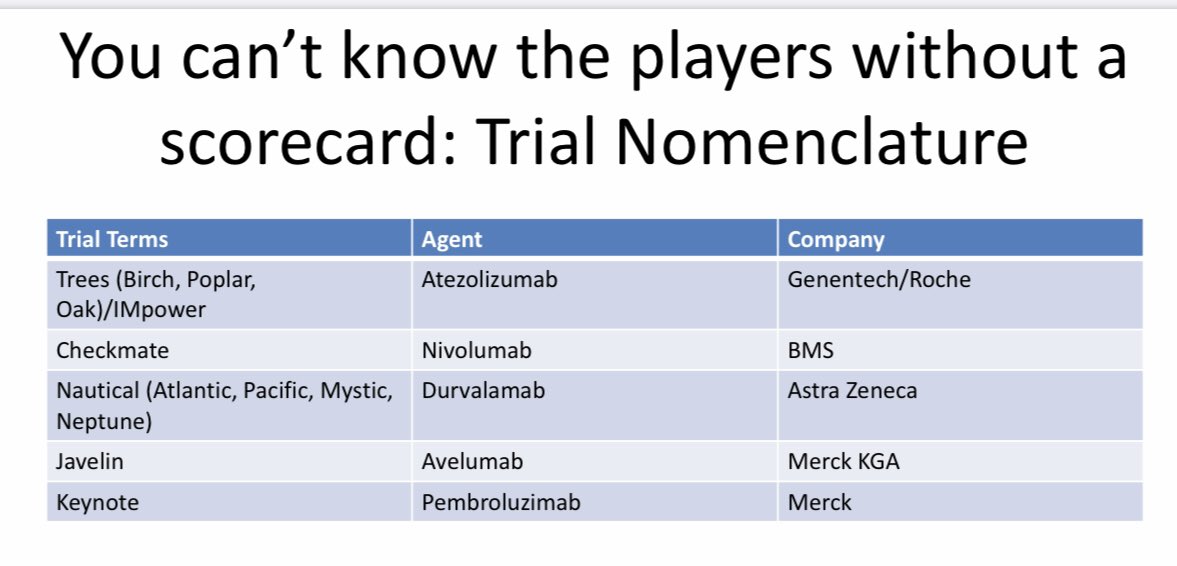
Q9. Immunotherapy comes with its own language and jargon. Part of this has to do with clinical trials. Pembrolizumab was shown to be effective in non-small cell lung cancer in a trial that was part of which series of cancer trials?
#Immunotherapy #io
The correct answer is Keynote. I love this handy guide to trial nomenclature by Dr. Edelman from @FoxChaseCancer
oncnet.com/sites/default/…
In extensive stage small cell lung carcinoma, the combination of carboplatin and etoposide chemotherapy has been standard of care for many years. Addition of which drug to this combo has been shown to increase overall survival?
The correct answer is atezolizumab (a PD-L1 inhibitor). The trial was IMpower133.
nejm.org/doi/full/10.10…
Q11. You have a patient with stage 4 lung adenocarcinoma with a targetable EGFR mutation but also PD-L1 more than 50%. What’s your best treatment option? (March 2020)
The answer is Osimertinib, at least at the current time. There is some evidence that immunotherapy may harm patients with driver mutations.
Also, Osimertinib is superior to other EGFR inhibitors in this setting (see FLAURA trial, below)
nejm.org/doi/full/10.10…
Q12. This is a fun question. Dr. Allison who discovered CTLA-4, did not like the name of its inhibitor, Ipilumumab. He jokingly suggested it be called Hippie-lumumab because of where it was discovered. Where was it discovered?
The answer is UC Berkeley, where Dr. Allison worked at the time.
The paper where he reported his findings is here 👇🏾👇🏾
crl.berkeley.edu/wp-content/upl…
Dr. Allison talks about his dislike for the name in this excellent video 👇🏾👇🏾
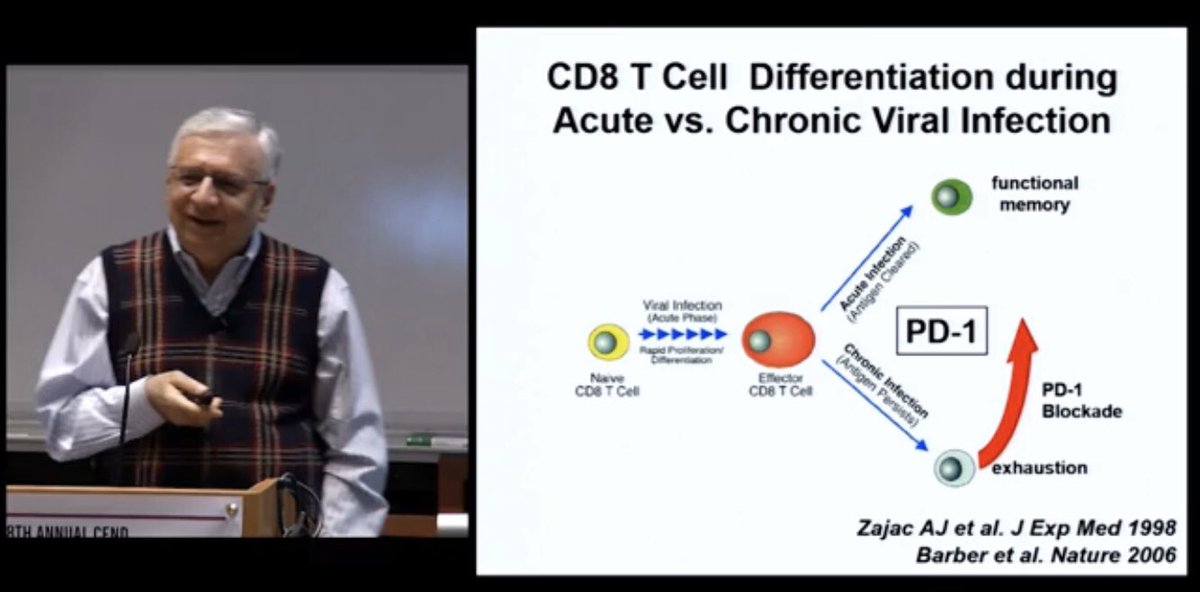
The T cells that try to kill PD-L1 positive tumor cells eventually fail and become functionally inactive. They remain in the vicinity of the tumor, however, waiting to be unleashed some day. They express PD-1, CTLA-4 and TIM-3. What are these T cells called?
They are called “exhausted” T cells. These cells are the ones unleashed by PD-1 and PD-L1 inhibitors
researchgate.net/profile/E_John…
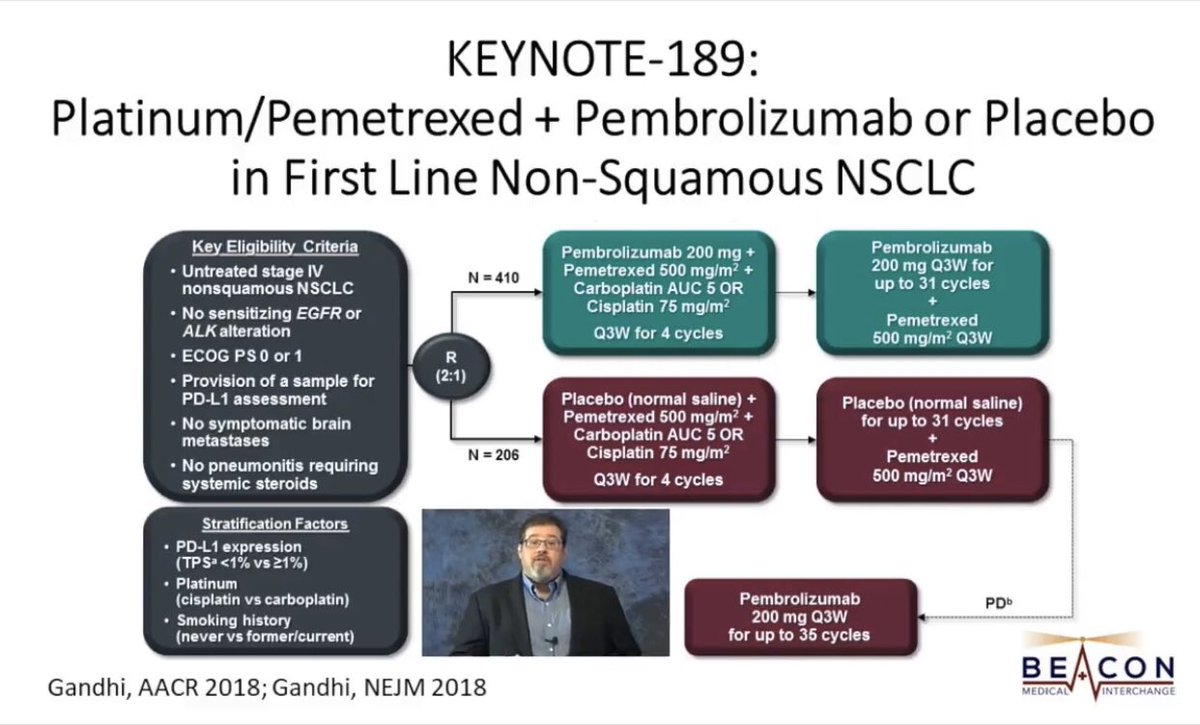
Q14. In 2018, a trial involving more than 600 patients showed that in advanced non-squamous driver-negative non-small cell lung carcinoma, chemo + pembrolizumab was better than chemo alone. The chemo backbone was platinum + pemetrexed. What was the trial called?
The answer is KEYNOTE-189. The implications of the trial are explained at great length by lung oncology guru @JackWestMD here 👇🏾👇🏾
Check out all the immensely educational videos and podcast by Dr. West if you are interested in lung cancer oncology!
Q15. The more the mutations in a tumor, the higher the neoantigens, the more likely that T cells will recognize tumor, and the higher the likelihood of benefit from checkpoint inhibitors. Which of the following has the lowest tumor mutational burden?
The correct answer is adenocarcinoma of the prostate. This tumor has low tumor mutational burden (TMB) in general, just like pancreatic adenocarcinoma.
The other tumors in the question have high TMB, and are therefore ideal candidates for immunotherapy.
@pembeoltulu
Q16. In 2017, a trial reported increased progression-free survival with durvalumab in the consolidation phase after completion of chemoradiation for stage 3 unresectable non-small cell lung cancer. Later, an overall survival benefit was also reported.
What’s the trial?
The trial is PACIFIC. Note that it involves immunotherapy in stage 3, as opposed to the usual setting (stage 4)
See excellent summary of the trial by oncologist @StephenVLiu here 👇🏾
See @NEJM paper here 👇🏾
nejm.org/doi/full/10.10…
Q17. Let’s see how well you know your immune checkpoint inhibitors (ICIs). They are grouped here in pairs according to what they inhibit (i.e., both drugs in a pair inhibit the same thing). Which pair is MISMATCHED?