Given recent news about prosecuting people across the UK for surviving suicide attempts, it's worth considering whether and when (if ever) clinical psychologists, psychiatrists and psychiatric nurses should endorse, encourage or incite prosecution as a clinical decision
Do the clinical benefits of clinical psychologists, psychiatrists & psychiatric nurses encouraging the prosecution of suicide attempt survivors outweigh the harms of doing so?
Death
Lifelong psychological harm
Criminal record
Loss of career
Financial loss
Family/relationship breakdown
Irretrievable loss of trust in MH staff leading to exclusion from treatment
Clinical/symptom outcomes
Patient experience of health services
Service use
Social/functional outcomes
Absolutely none
Level 3 institutional abuse
Level 1 - direct abuse of patients by individual staff (verbal/emotional/physical/sexual etc)
Level 2 - abusive regimes (enabling level 1 abuse / deliberate & vexatious exclusion etc)
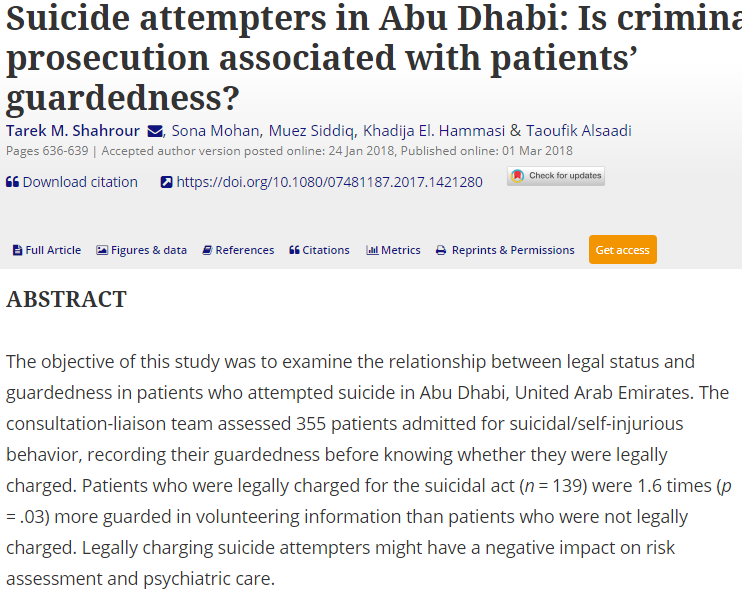
1 This is true, in at least a robust observational study
2 It is not occurring at the expense of wellbeing or clinical symptoms
Employment
Housing
Relationships
Raising children
Does the encouragement of prosecution for attempting suicide improve security of housing?
Does the encouragement of prosecution for attempting suicide keep families together?
en.m.wikipedia.org/wiki/Breach_of…
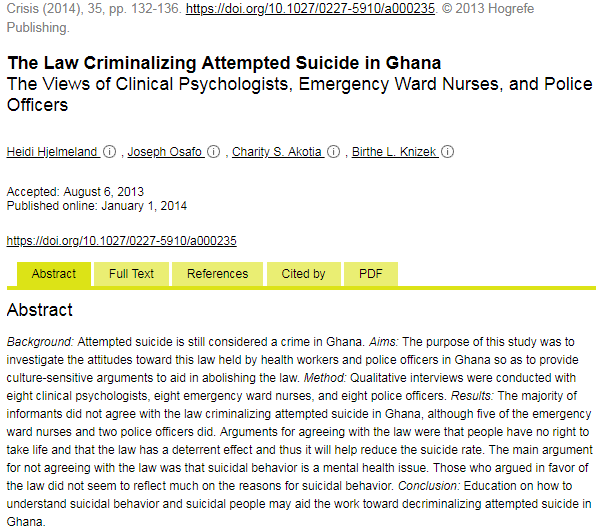
There is no reported clinical benefit
There are substantial known & demonstrable harms
Death
Lifelong psychological harm
Criminal record
Loss of career
Financial loss
Family/relationship breakdown
Irretrievable loss of trust in MH staff leading to exclusion from treatment
In health care this is done all the time: aortic aneurysm repair, cancer surgery, many drug treatments etc.
No
Is there evidence of harm?
Yes
Do we know the rate of harm?
No
Can we justify this intervention on the grounds of benefits outweighing harms?
No.
This is a matter for the police & courts. As a CP, Dr or nurse, if you opine on culpability you are outside the bounds of both your competence & ethics, thereby jeopardising your professional registration
Unless you can demonstrate:
1 A robust theoretical framework
2 Evidence of benefits which vastly outweigh the harms
...this amounts to nothing more than pseudopsychoanalytic theorising & again you are jeopardising your professional registration
This is squarely outside the ethics & standards frameworks of the HCPC, NMC & GMC. It is very close to moral judgement & advocating punishment- not the professional role of a CP, Dr or nurse
We have already established that prosecution has no benefits & substantial harms. If commissioners or MH staff are excluding a person from help, it is those people who should be prosecuted, not their patient
when (if ever) is it clinically justified for clinical psychologists, psychiatrists and psychiatric nurses to endorse, encourage or incite prosecution for offences associated with attempting suicide or being suicidal?
Given that the harms are substantial, permanent or even fatal
Given that other considerations are outside the ethics &duties of clinical psychologists, psychiatrists & psychiatric nurses
The answer is "Never"