Here's how.
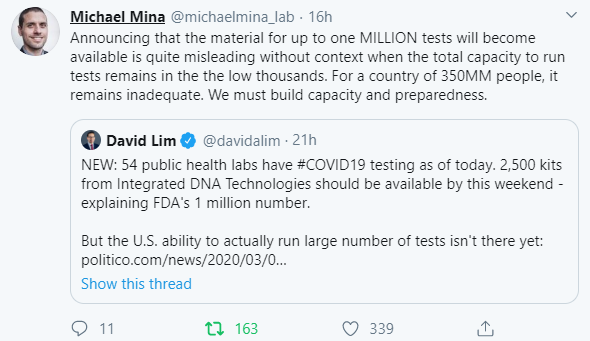
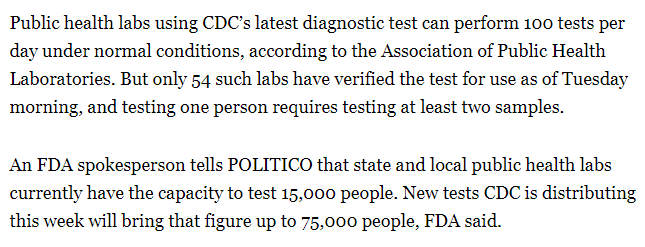
As @JenniferNuzzo laid out clearly yesterday, there are a finite number of public health workers, and where the government opts to focus their attention is a major strategic choice.
The administration chose to put almost all its eggs into the containment basket. And that policy choice comes through clearly in this woman's experience.
This should have been in the works from the moment we saw the case volumes being generated in Wuhan.
Most people will turn first to their primary care doc or an urgent care clinic if they get sick. Ensuring those facilities are informed and equipped to handle a surge in questions - didn't happen.
This case suggests the website guidance isn't translating into practice.
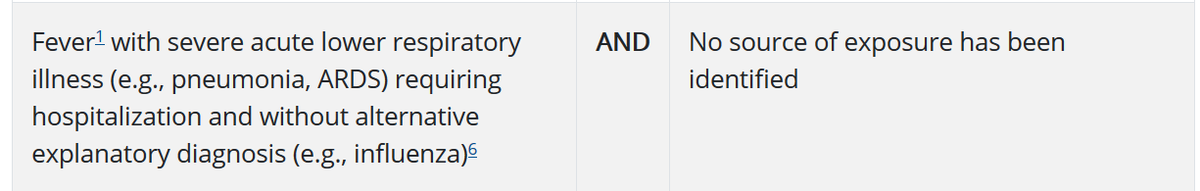
CDC's testing criteria expanded last week to include potential community spread - hence the nationwide jump in case identification this week. But as this instance shows, it's still too narrow.
That's a problem because 80% of cases (and thus, spreaders) don't reach this level of severity. So remain invisible.
cdc.gov/coronavirus/20…
But there's one more breakdown: frontline hospital readiness.
As writer notes, she won't be able to get testing unless/until she ends up in the ER.
That was a month and a half ago, and yet we're still unprepared.
But that turned out to be an absence-of-evidence ≠ evidence-of-absence issue. The lack of cases reflected nothing more than the artificial narrowness of their testing criteria.
There's a clear line between high level policy choices made in the White House and a symptomatic individual potentially endangering others because she can't get tested.
@_b_next @UNMCCOPH jointly issued last month: