Hope everyone can join!
This will pair very well with @CardioNerds Episode #20 on COVID in the ICU: cardionerds.com/episodes/covid…
🧐Why is there heart failure?
- hypoxic injury? myocarditis?
But clincial presentation with heart failure and hypotension seems out of proportion...why?
But many questions remain..
- why proBNP and TnI elevation?
- why d-dimer elevated?
- best treatment plan?
- role of anti-inflammation Rx?
Ongoing study of Tocilizumab, anti-Il-6 Ab.
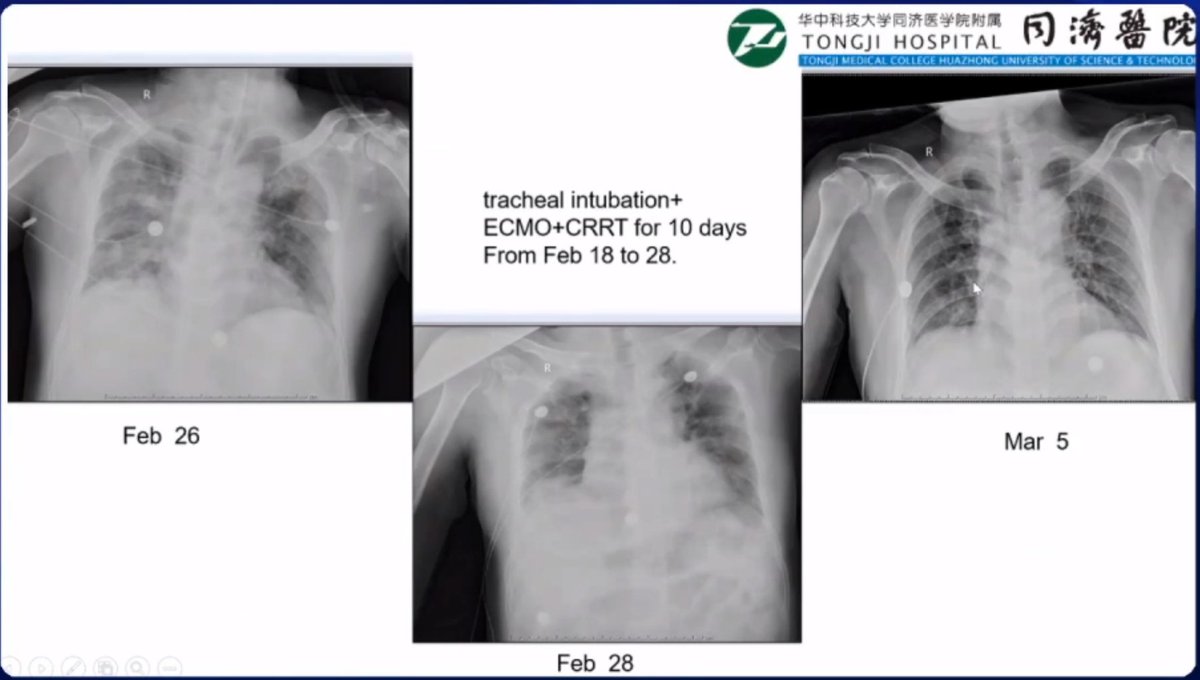
4 recovered, 1 ongoing
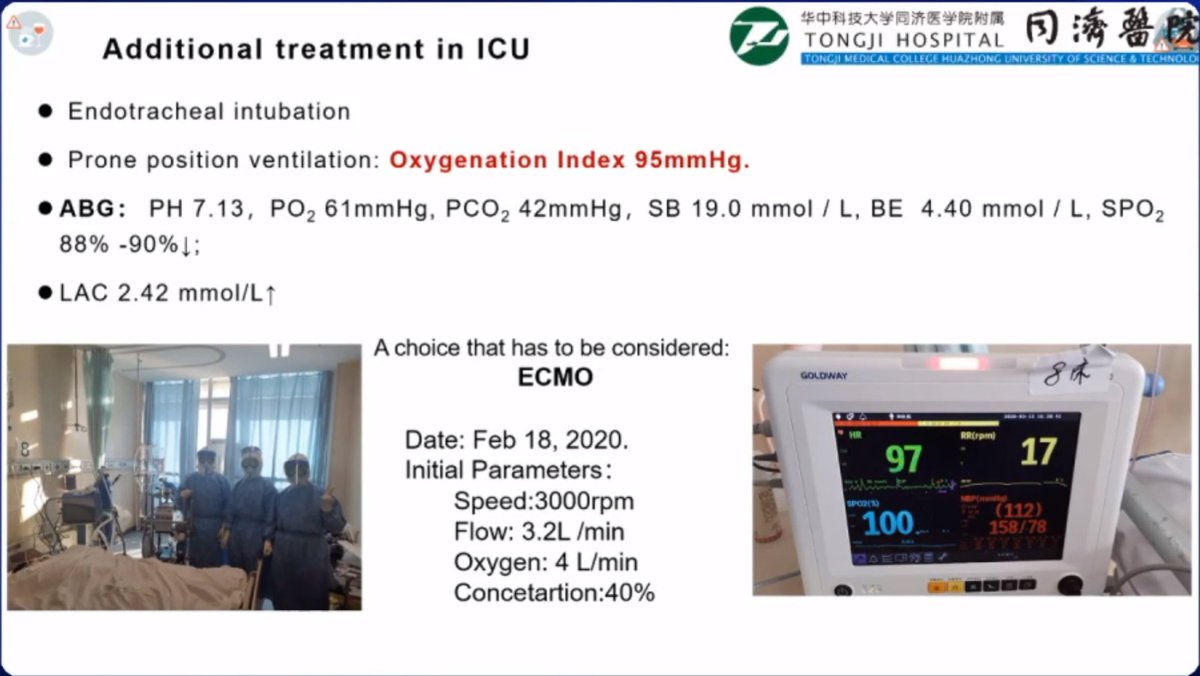
4 VV-ECMO, 1 VA-ECMO
Duration ~9.2 days, range 6-13 days
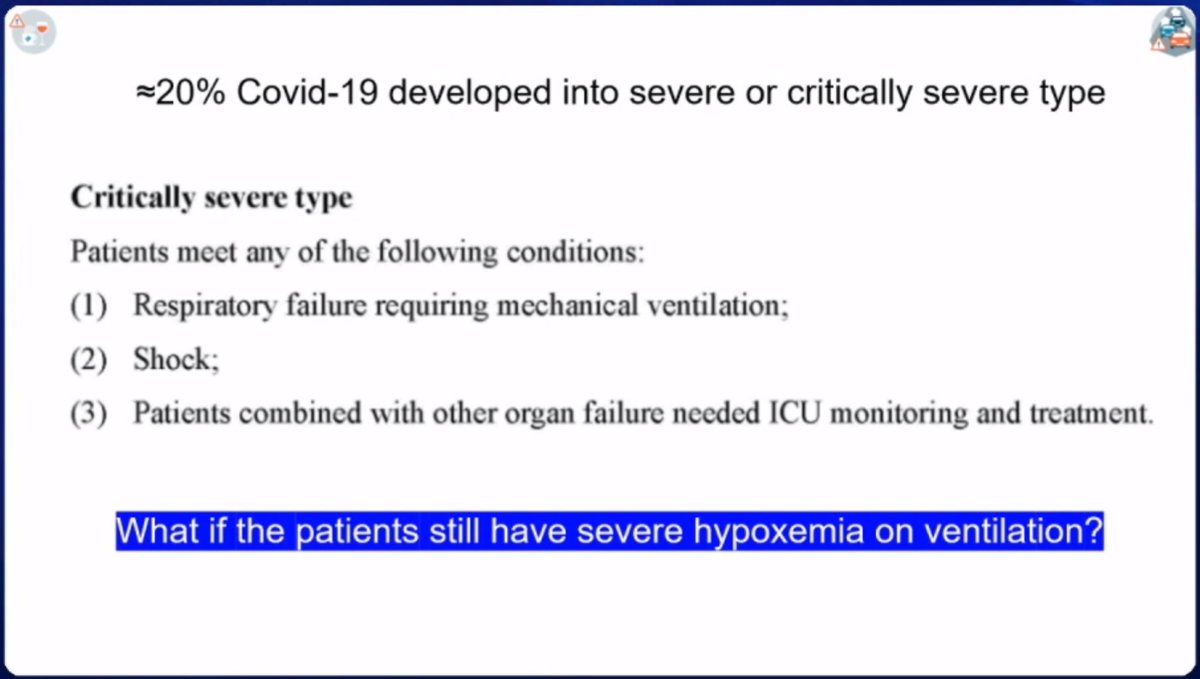
✅Indications:
- not standard, don't wait for last resort
- need to lower threshold
- don't wait for severe hypoxia which leads to multiorgan failure
- don't do ECMO when patient is dying
- bleeding (need anticoagulation)
- irreversible severe brain injury
- poor outlook: deathly ill, advanced age
Don't have ECMO for everyone...we have to choose patients who are more likely to recover
- earlier is probably better, if progression is ominous
- if wait too long, may loose the chance to recover them
- ECMO is not just to prolong life for couple days...want to use for SURVIVAL 👏
1st is VV-ECMO - for severe respiratory failure not responding to mechanical ventillation
BUT if cardiac dysfunction 💔 --> don't forget they may need a VA-ECMO
- risk of transmission
- resource limitation
- interrupts airway clearance
Is there a place for VV-ECMO without intubation⁉️
Hmmm...🤨
Something maybe worth considering.
...they are the heros of my city" (Wuhan, China)
-Not all 🏥have ECMO...limited availability
-Most often using VV-ECMO <-- hypoxemia is #1⃣
-VA-ECMO: ⏫Afterload > bad for ♥️
-BUT: if heart failure 💔 & Hypoxia
--> VA-ECMO + Impella
Is there a way to identify the sickest?
Ans:
- no risk score; clinical judgement
- oxygen, lactate, liver & kidney function
A: CRP (+/-cytokines) & cardiac biomarker
- severe, non-critical: once per week
- ICU patient: every 2-3 days
- severe critical: daily
A:
- Steroids: active debate in our group
- Possible benefit: may help reduce inflammatory storm
- Possible harm: prolong viral shedding, etc
- Not using commonly