First, a question. Which of the following play a role in the decrease in albumin concentrations in inflammatory conditions?
[TER = transcapillary escape rate]
If the decrease in albumin were due to decreased synthesis alone, its long half-life (~20 days) would mean that a substantial drop would not occur for days.
And yet, albumin sometimes decreases within HOURS of injury.
Something else must be going on.
ncbi.nlm.nih.gov/pubmed/2858667
Albumin has a baseline transcapillary escape rate (TER) of 5% per hour (i.e., 5% of albumin leaves the vascular space into tissues every hour).
In septic shock or after surgery, the TER increases within hours. This explains the early fall in albumin.
ncbi.nlm.nih.gov/pubmed/2858667
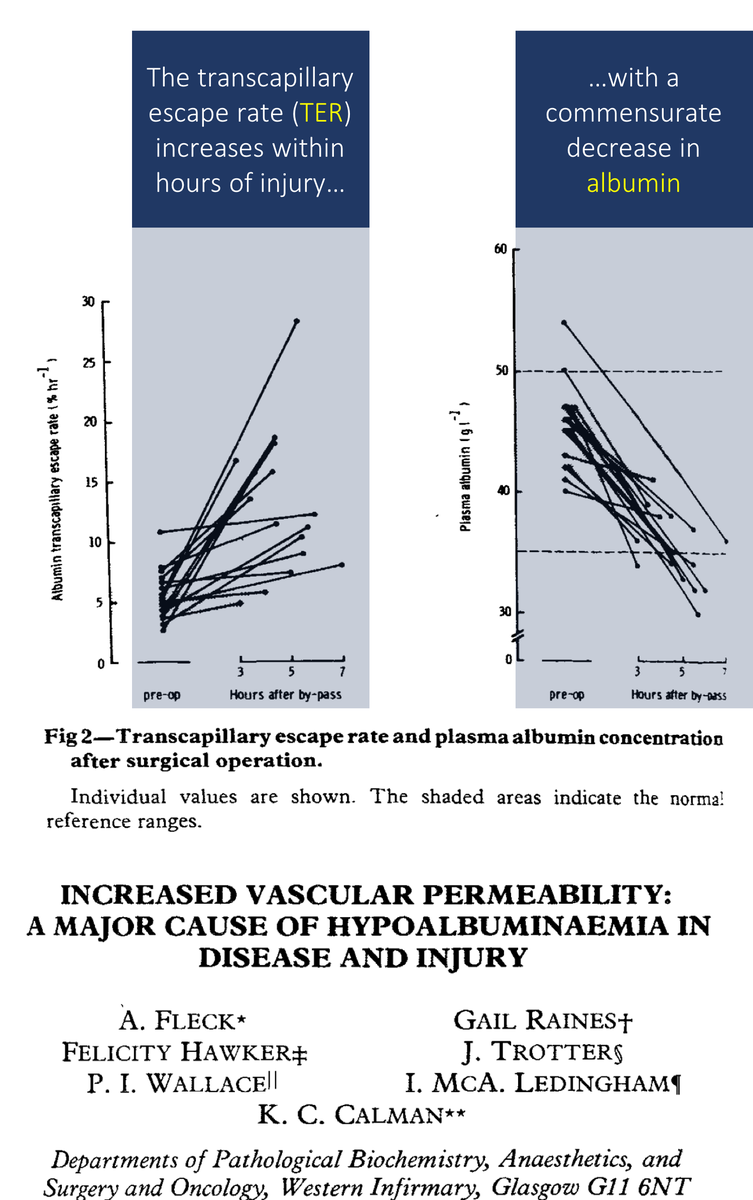
While increased catabolism also plays a role, most of the drop in albumin after the first day is likely due to decreased synthesis.
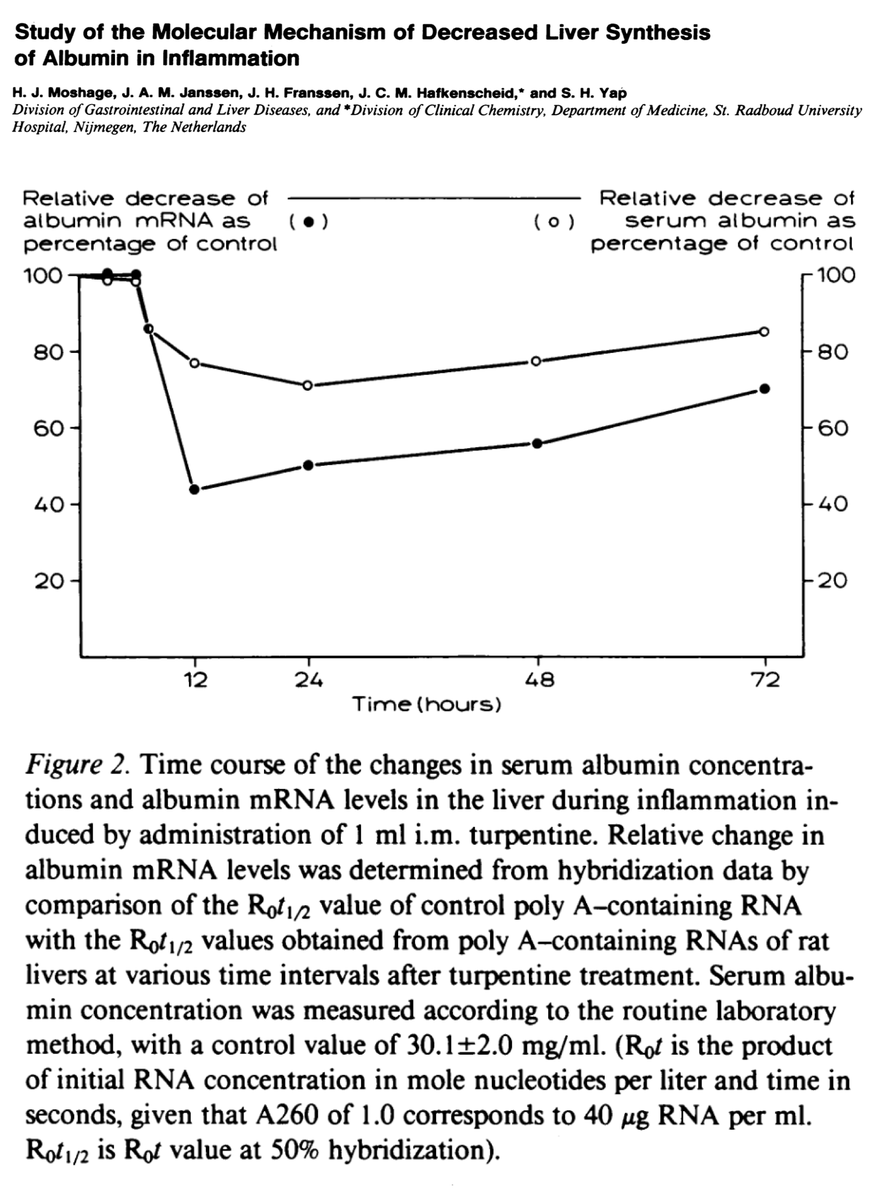
This was suggested in 1987 by Moshage et al who showed that albumin mRNA in livers decreased after acute inflammation.
ncbi.nlm.nih.gov/pubmed/3584463
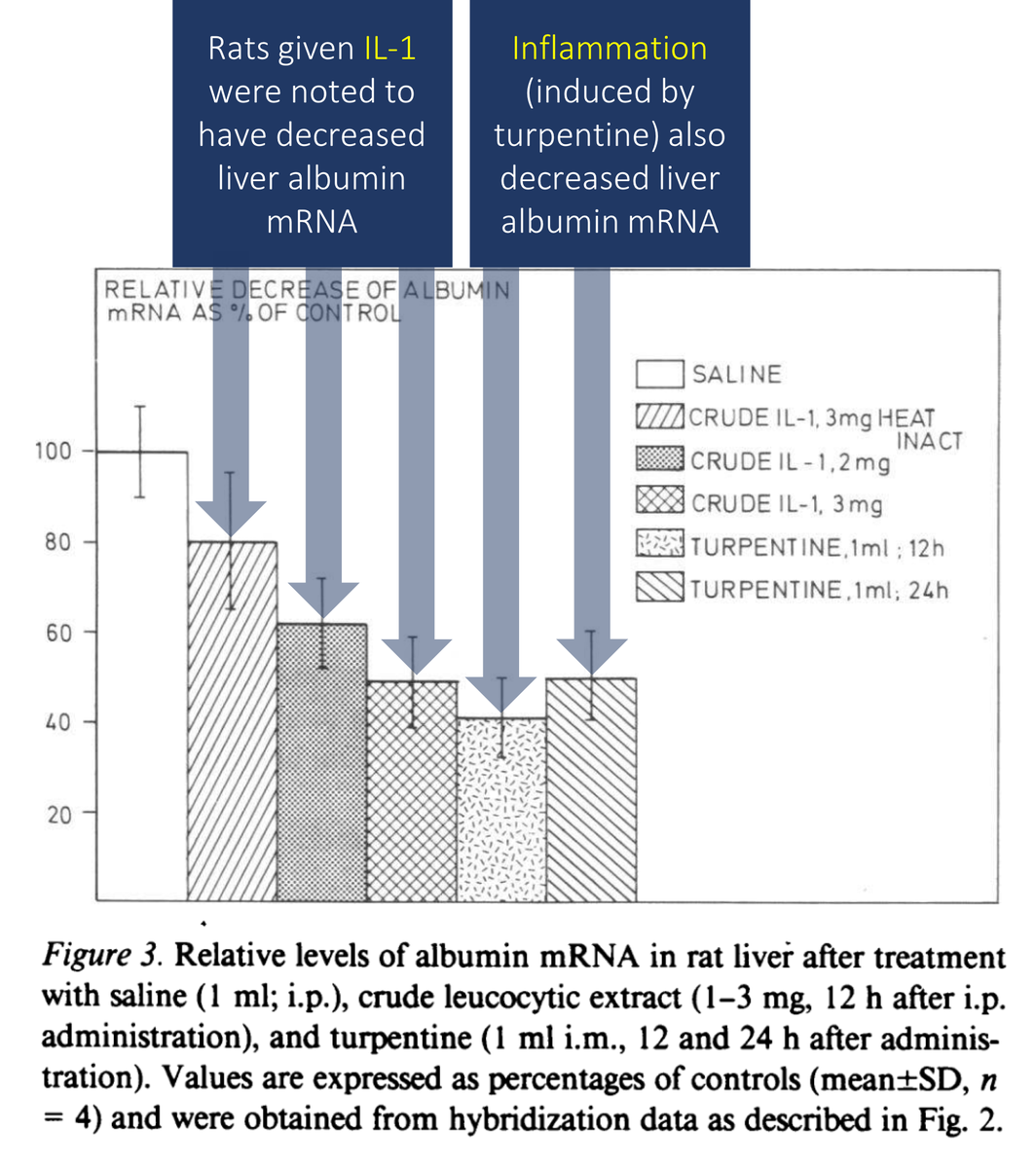
And what caused this decreased in albumin mRNA?
This same study suggested that IL-1 plays a role, likely alongside other cytokines associated with the acute inflammatory process. It seems as though the positive APR and negative APR are coordinated.
ncbi.nlm.nih.gov/pubmed/3584463
While all of the above helps demonstrate "how" albumin levels fall in inflammatory conditions, none of the above answers "why" albumin decreases.
Let's address this next.
What is your hypothesis? What is the benefit of decreasing albumin synthesis?
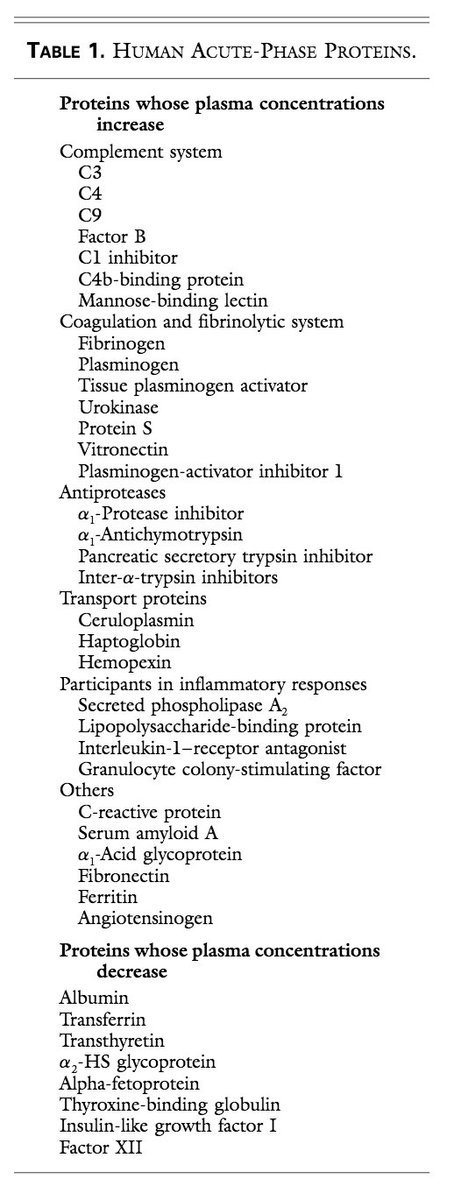
To understand why albumin is a negative acute phase reactant (APR), it is first helpful to review the role of positive APRs.
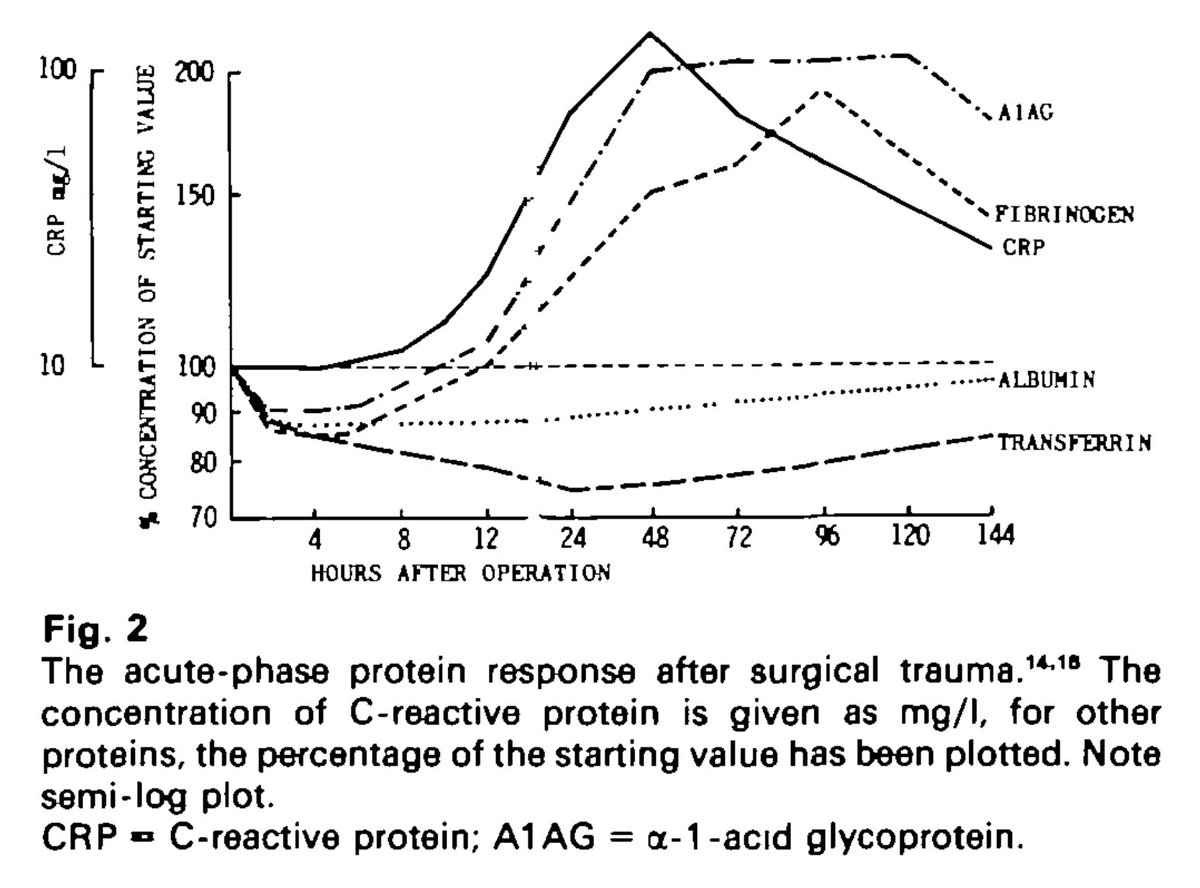
I'll cover two key examples: C-Reactive Protein (CRP) and fibrinogen.
ncbi.nlm.nih.gov/pubmed/9971870
Amazingly, CRP can increase 1000-fold in acute inflammation!
Regarding its role, CRP has multiple functions, including activation of complement and aiding is opsonization and clearance of necrotic and apoptotic cells.
It isn't just a lab test...
ncbi.nlm.nih.gov/pubmed/12384129
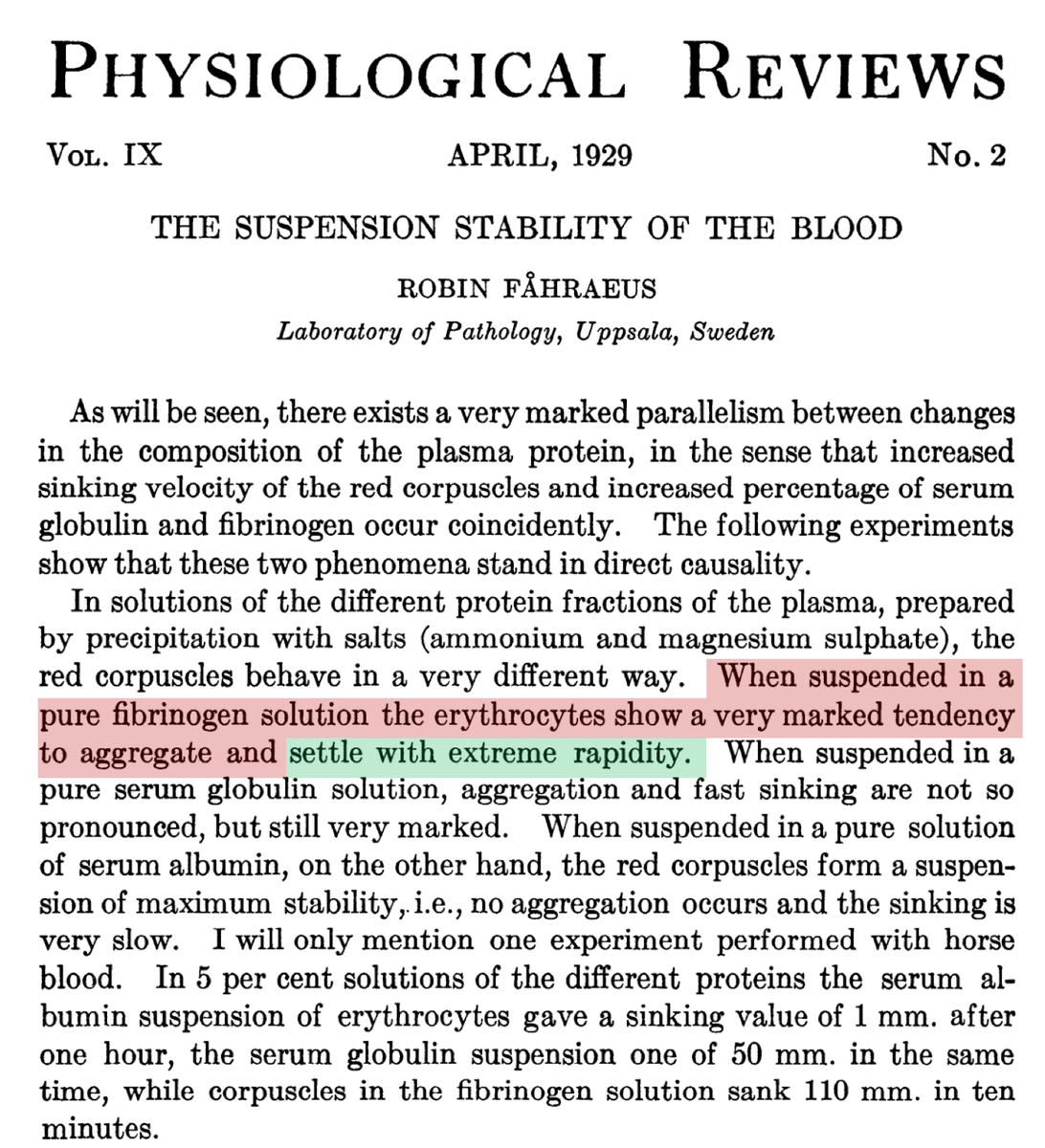
Fibrinogen is critical to tissue repair resulting from inflammation as it causes endothelial cell adhesion, spreading, and proliferation.
But, we don't usually measure fibrinogen. Instead, we use a surrogate test...
...ESR!
ncbi.nlm.nih.gov/pubmed/4014259
RBCs are negatively charged. As a result, they repel each other.
Fibrinogen is positively charged and is an absorbing force. This manifests as Rouleaux on a smear and increased ESR.
The effect of fibrinogen on ESR has been known since the 1920s!
physiology.org/doi/abs/10.115…
There are dozens of other positive APRs with myriad functions. They:
*cause adhesion and chemotaxis of phagocytic cells and lymphocytes (e.g., serum amyloid A)
*act as antioxidants (e.g., haptoglobin)
*scavenge iron (e.g., hepcidin)
ncbi.nlm.nih.gov/pubmed/9971870
This brings us back to albumin. Why would the concentration of albumin decrease in acute inflammation?
A clue comes from another name for acute phase reactants. They are also known as acute phase PROTEINS.
While not proven, some postulate that the fall in albumin occurs so that the body can appropriate amino acids to the acute phase proteins required in infection, trauma, etc.
Given that albumin is bountiful and (less) essential, it's synthesis falls.
How cool is that!
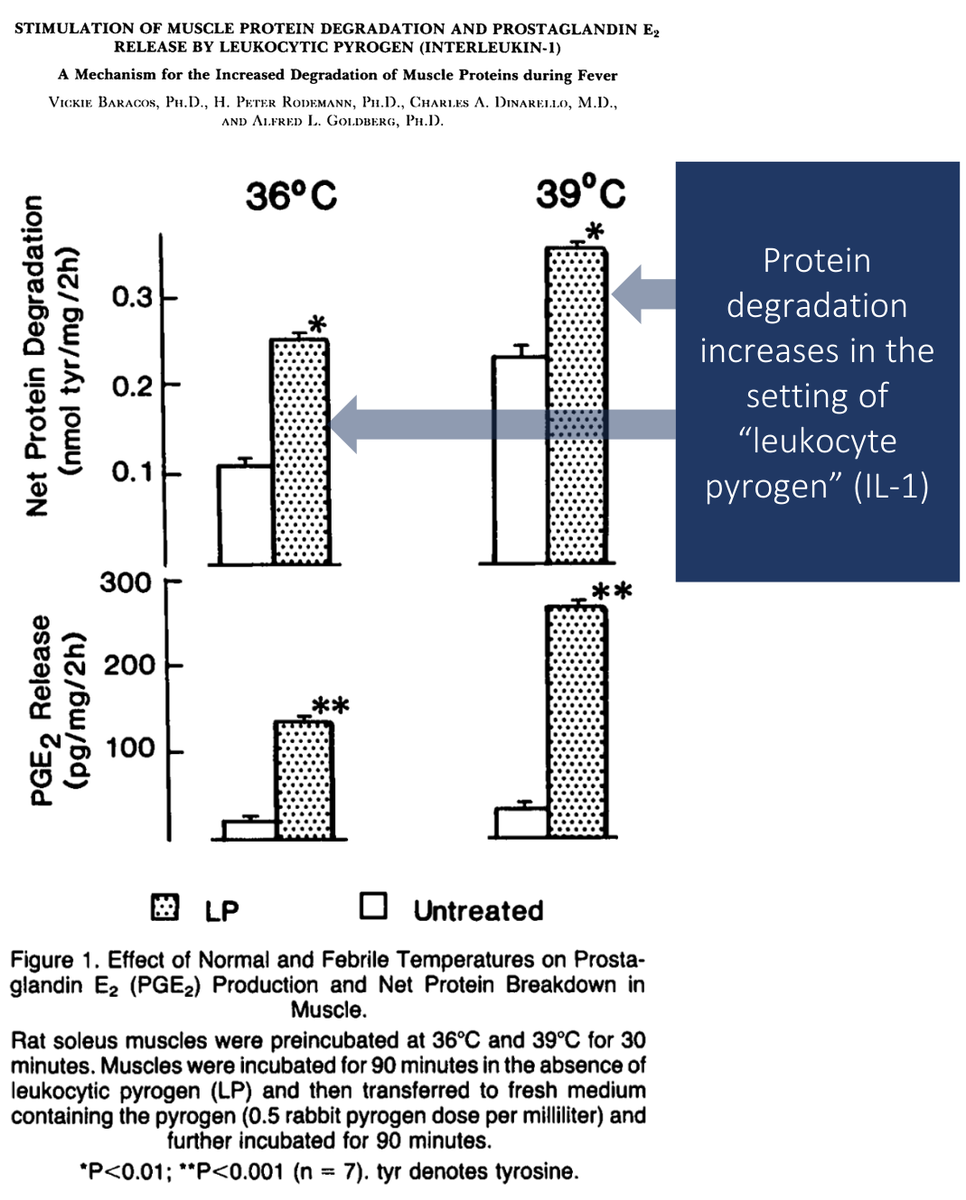
This need for more amino acids may also be part of the reason why inflammatory conditions lead to muscle catabolism.
Skeletal muscle is a great source of amino acids for immunoglobulin and positive APRs.
ncbi.nlm.nih.gov/pubmed/6402699
Before summarizing, let's ask the original question one more time.
Which of the following play a role in the decrease in albumin concentrations in inflammatory conditions?
[TER = transcapillary escape rate]
In summary:
⭐️albumin's decrease in inflammation is via
⬆️ TER (short-term);
⬆️ catabolism;
⬇️⬇️ synthesis
⭐️postive APR are proteins with myriad functions
⭐️albumin's role as a negative APR may be to provide amino acids for positive APR (and other proteins)