onlinecjc.ca/retrieve/pii/S…
In light of that article I thought I'd expand on the previous tweetorial.
@CAEP_Docs @UBCDoM @Vadeboncoeur_Al @CANet_nce @BCEmergMedNtwrk onlinecjc.ca/article/S0828-…
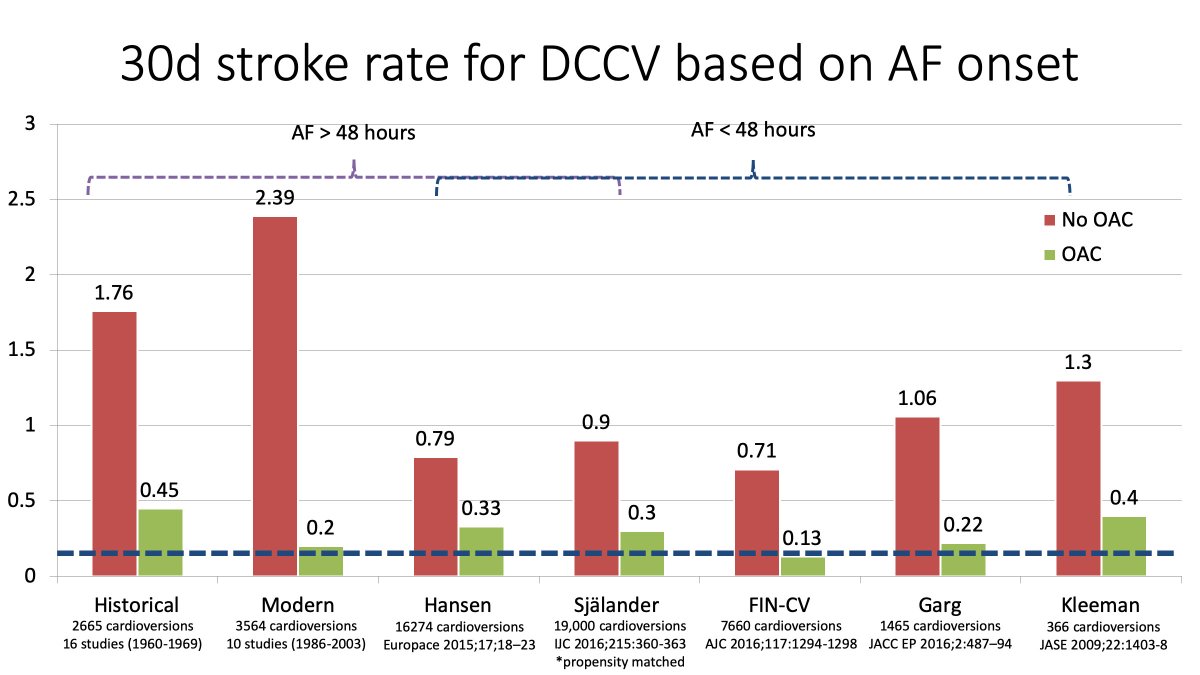
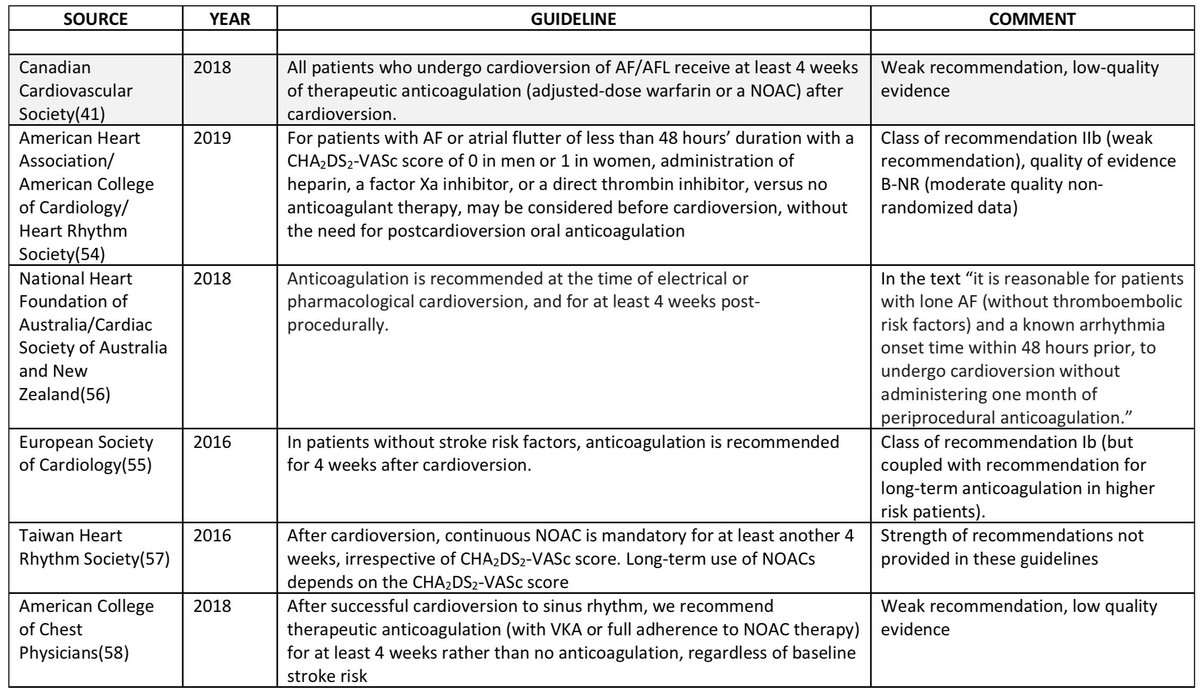
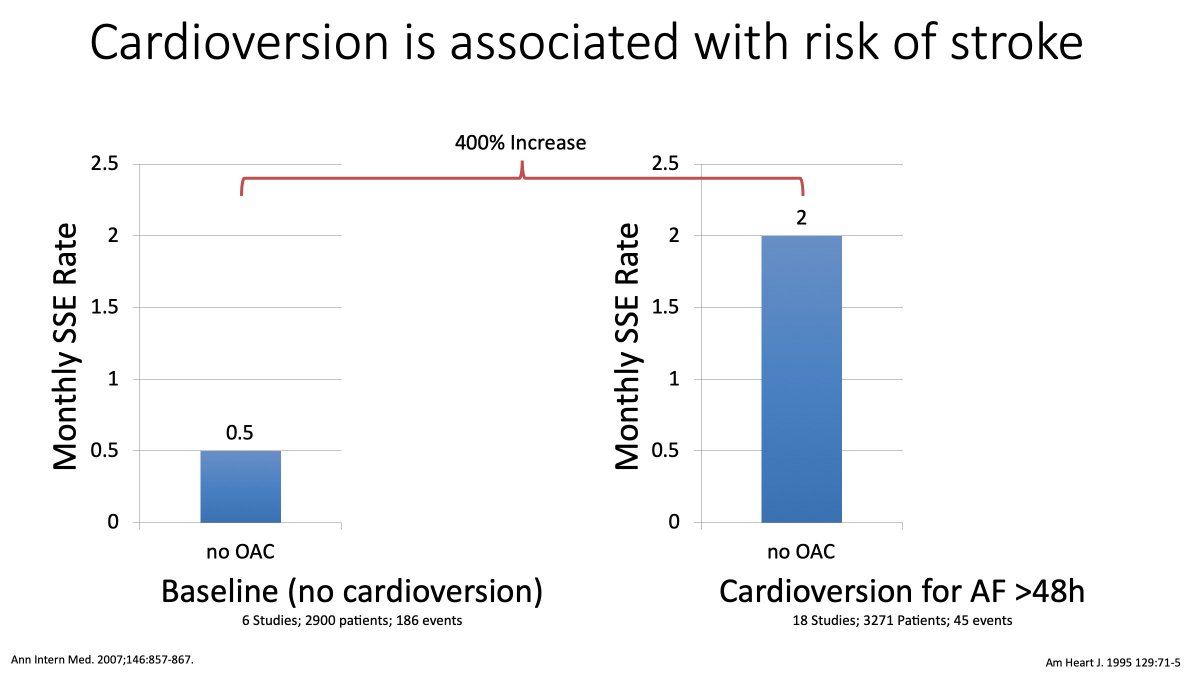
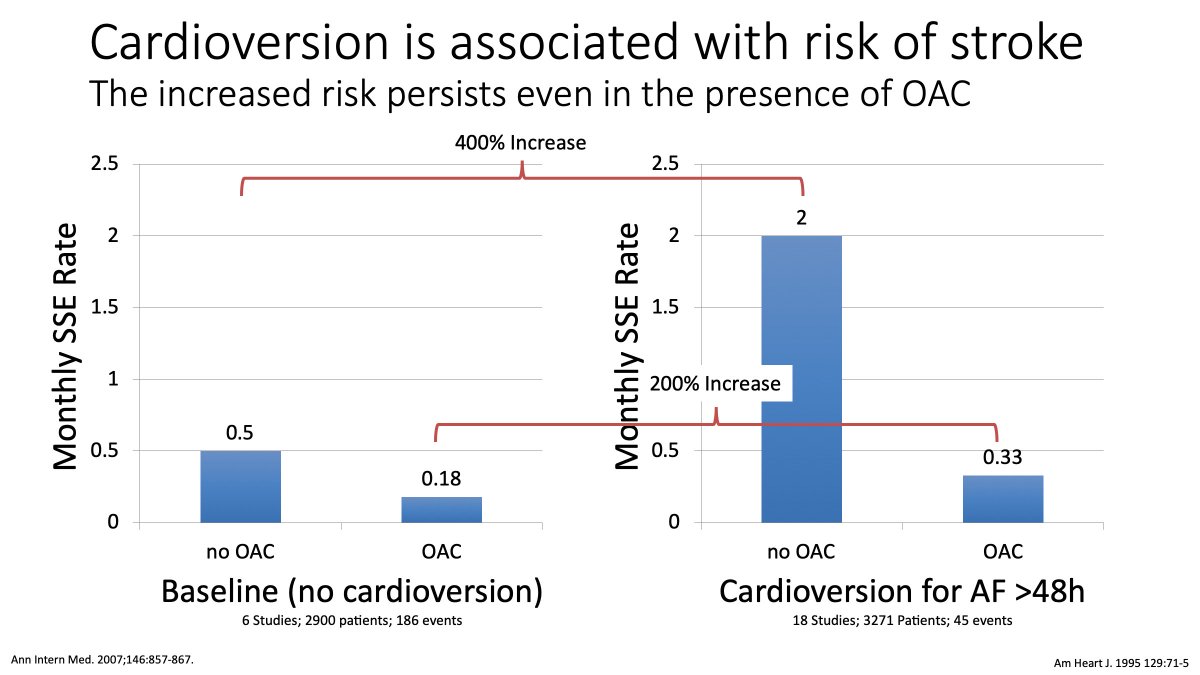
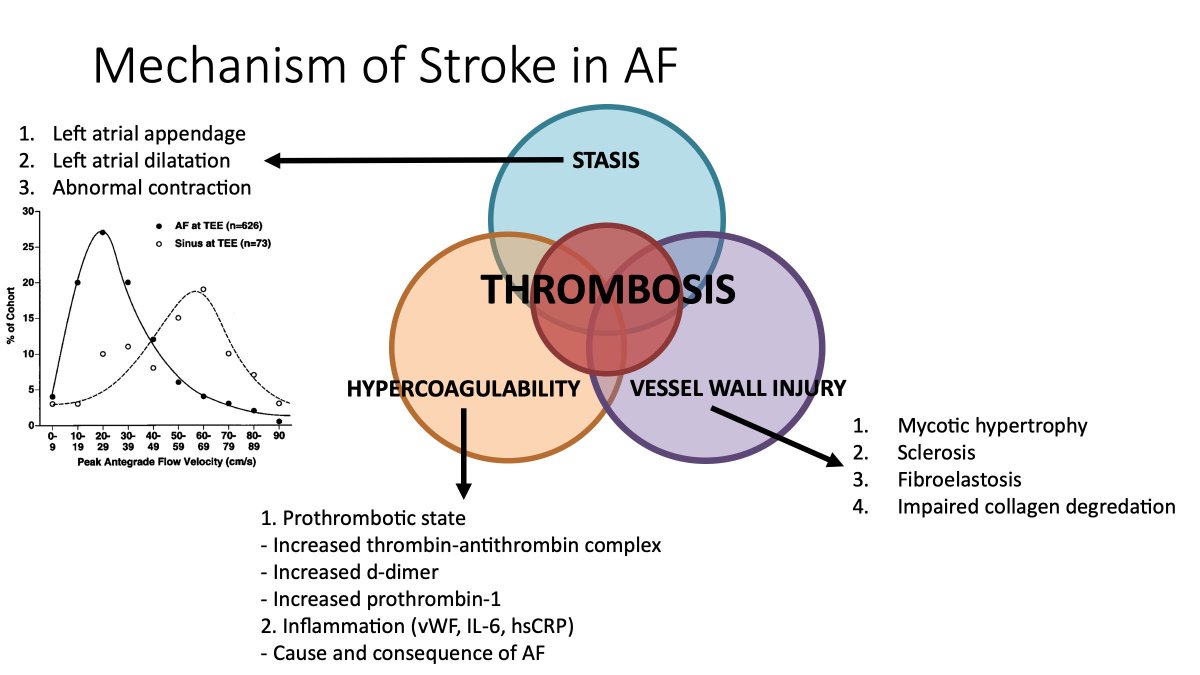
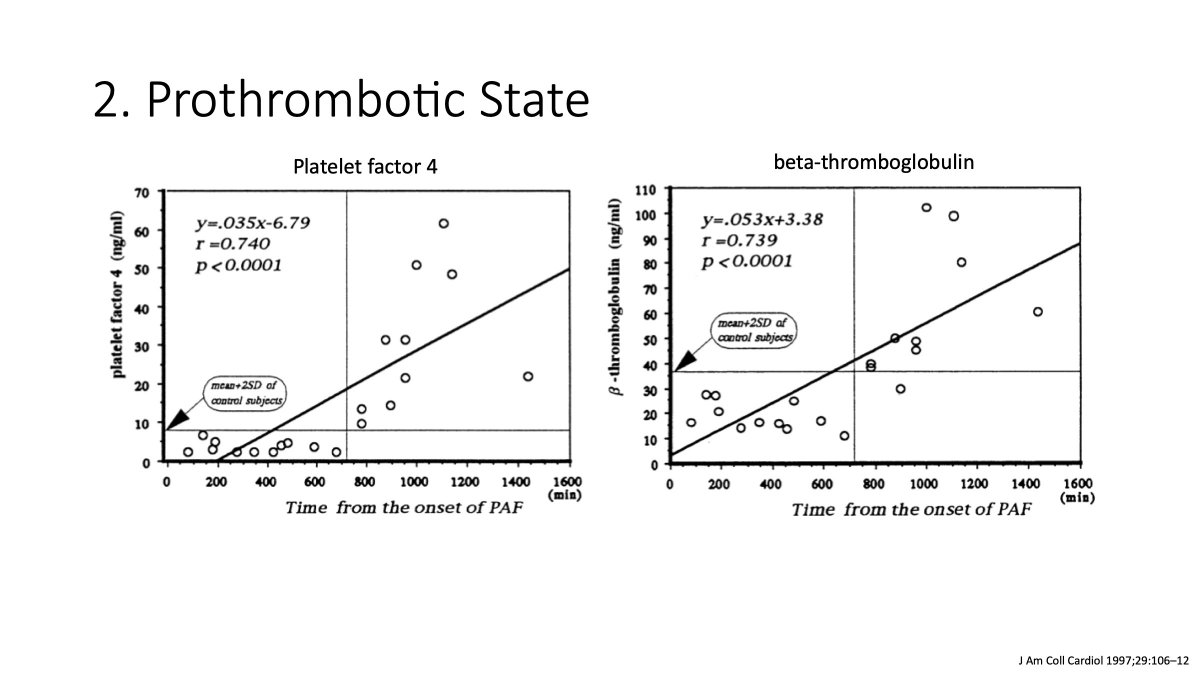
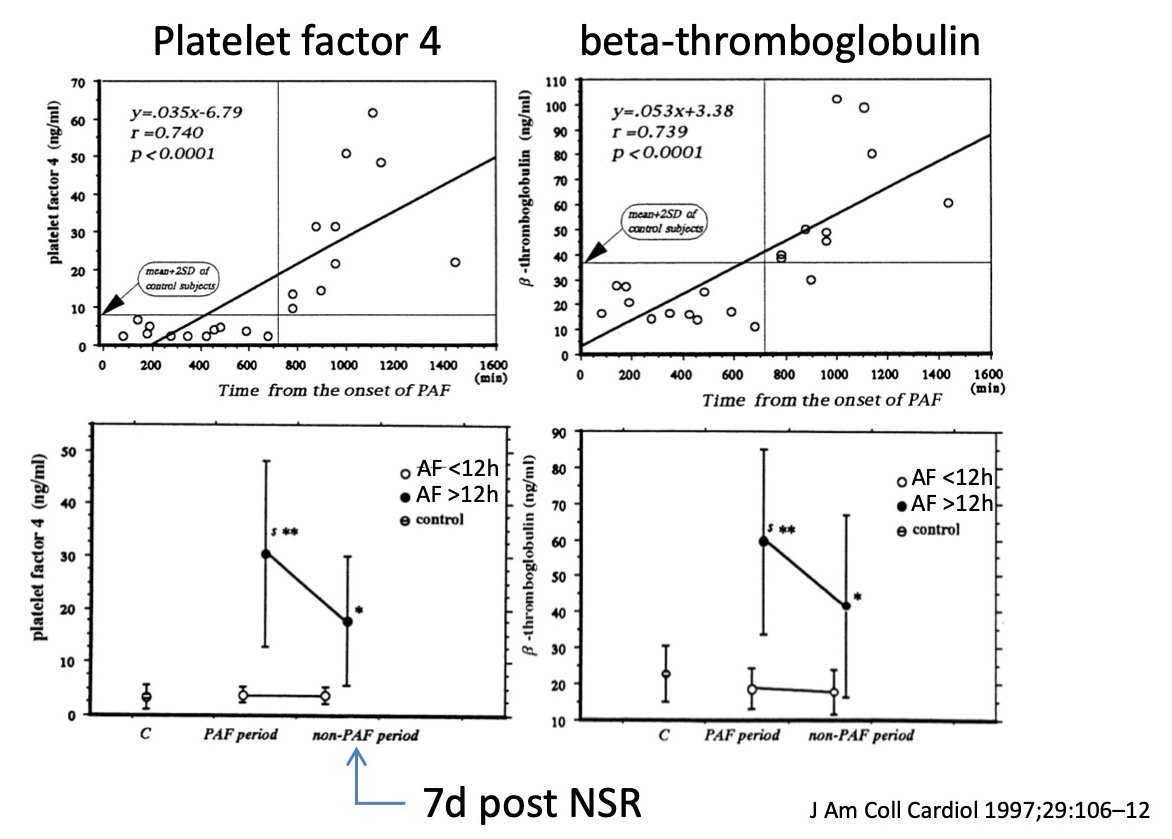
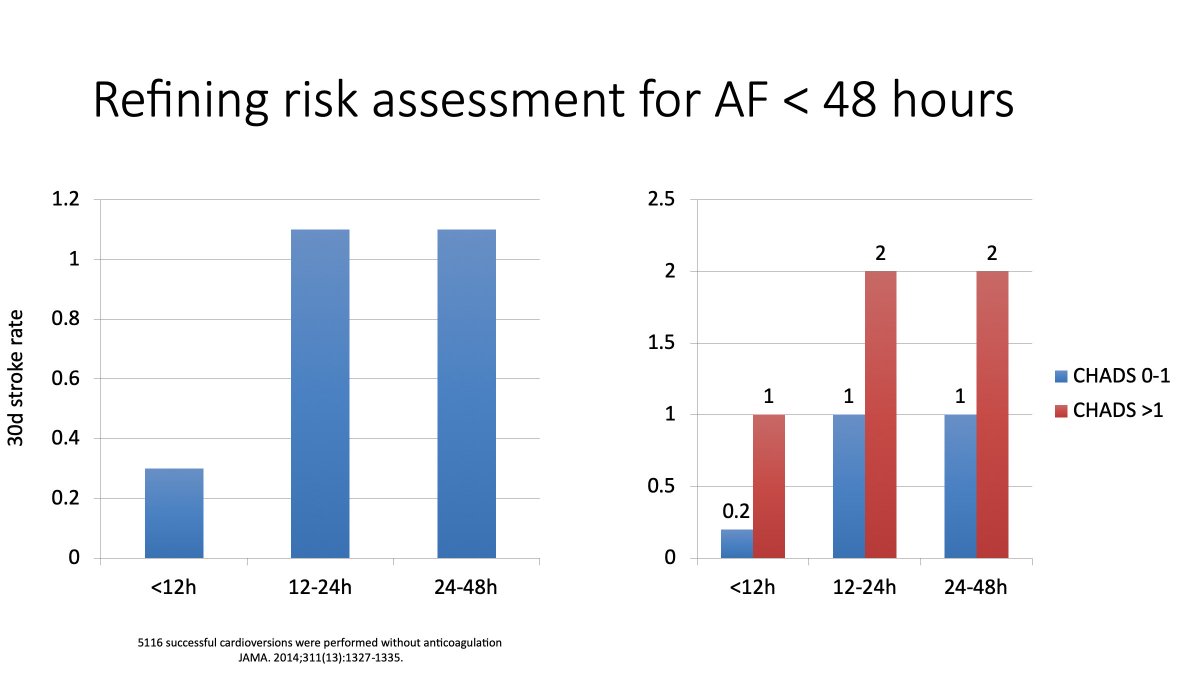
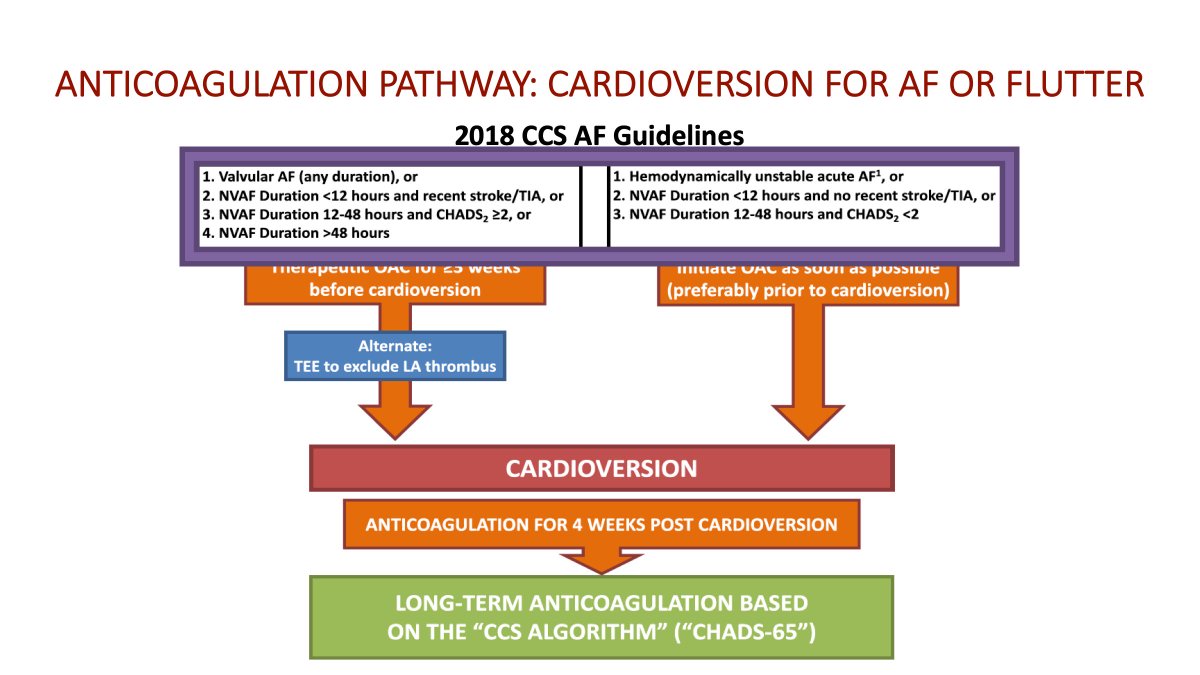
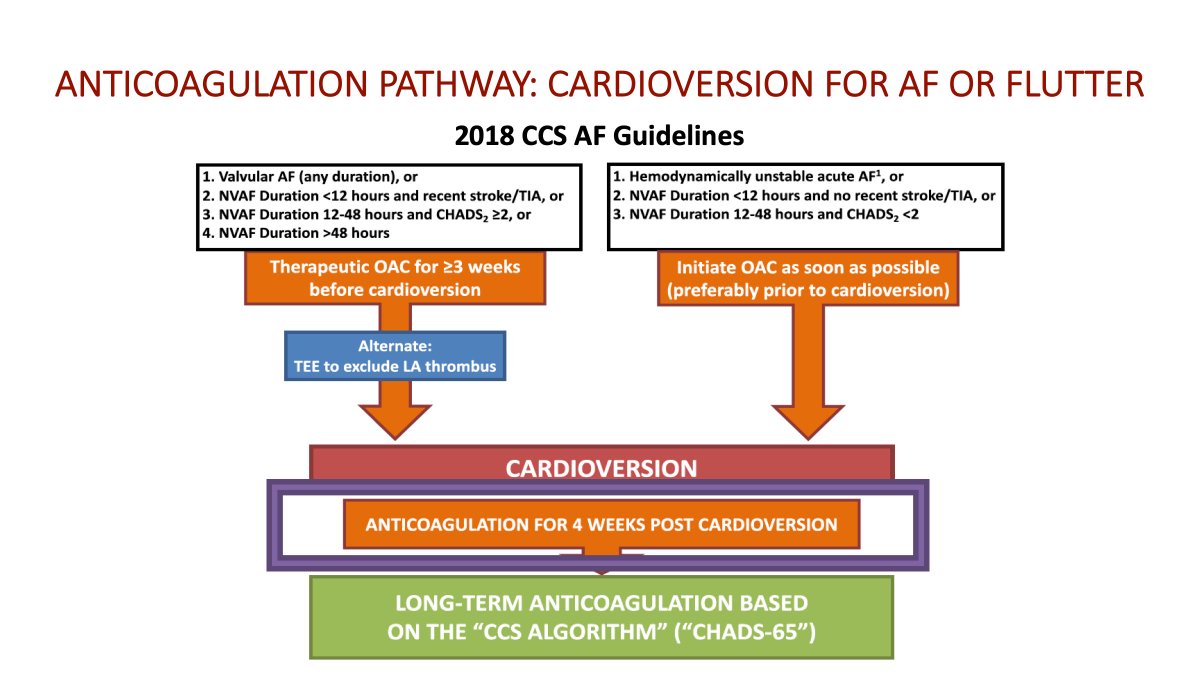
We use the 12 hour threshold for patients with risk factors.
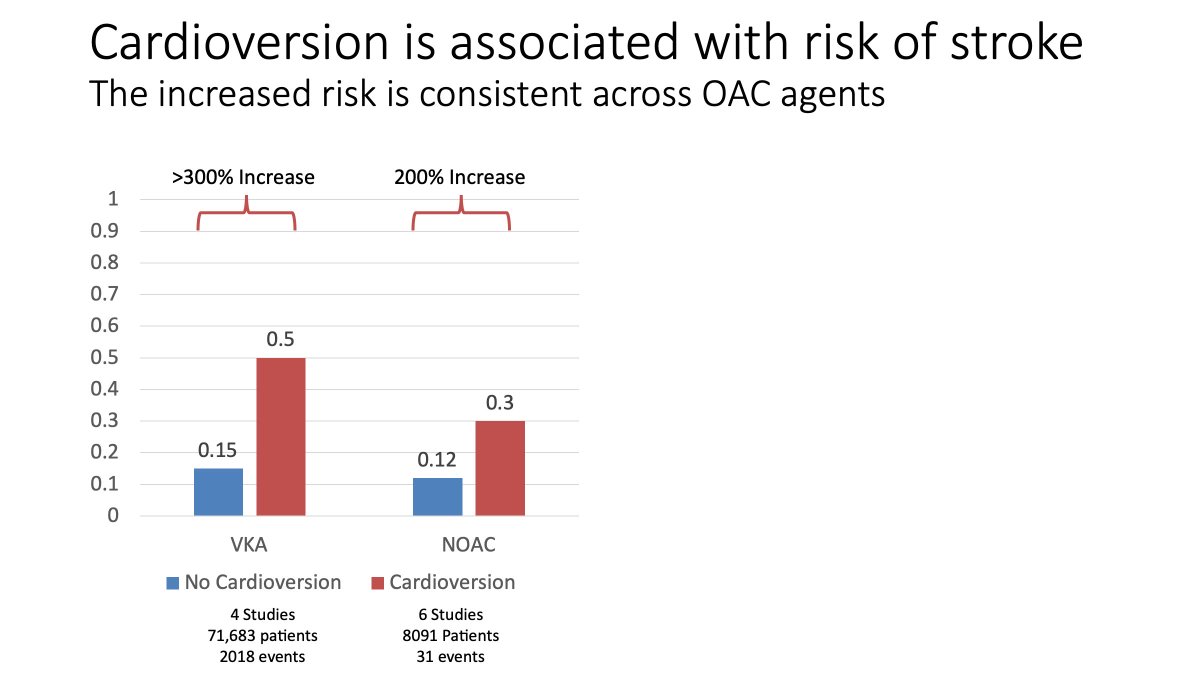
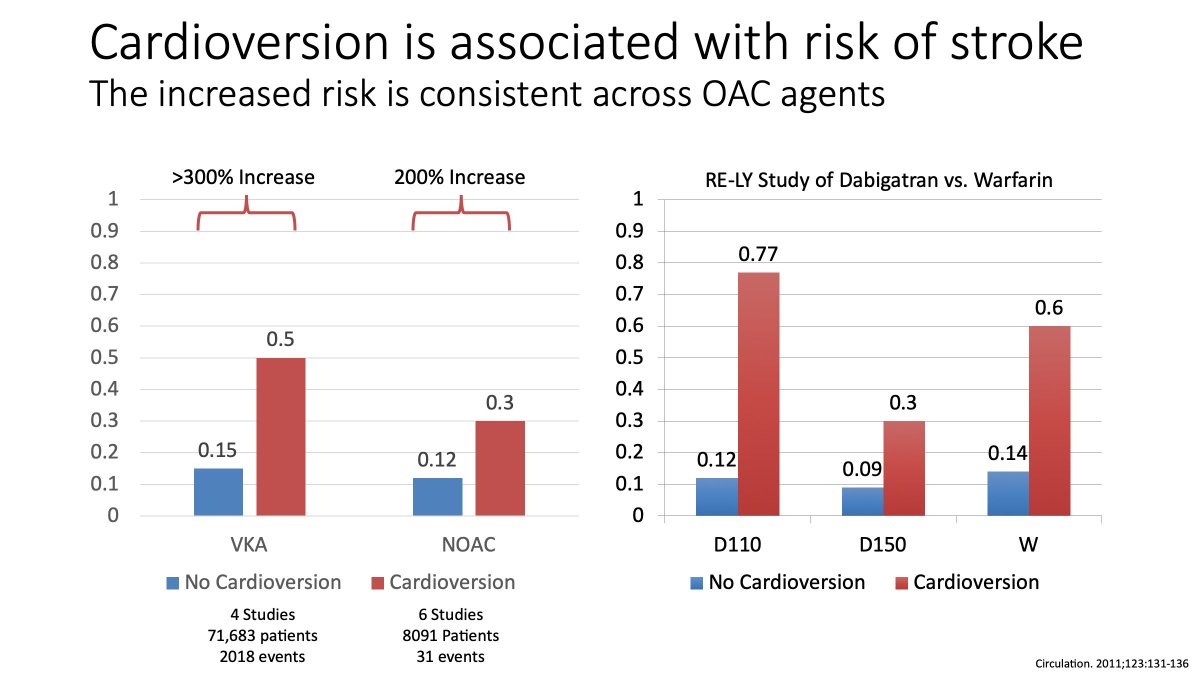
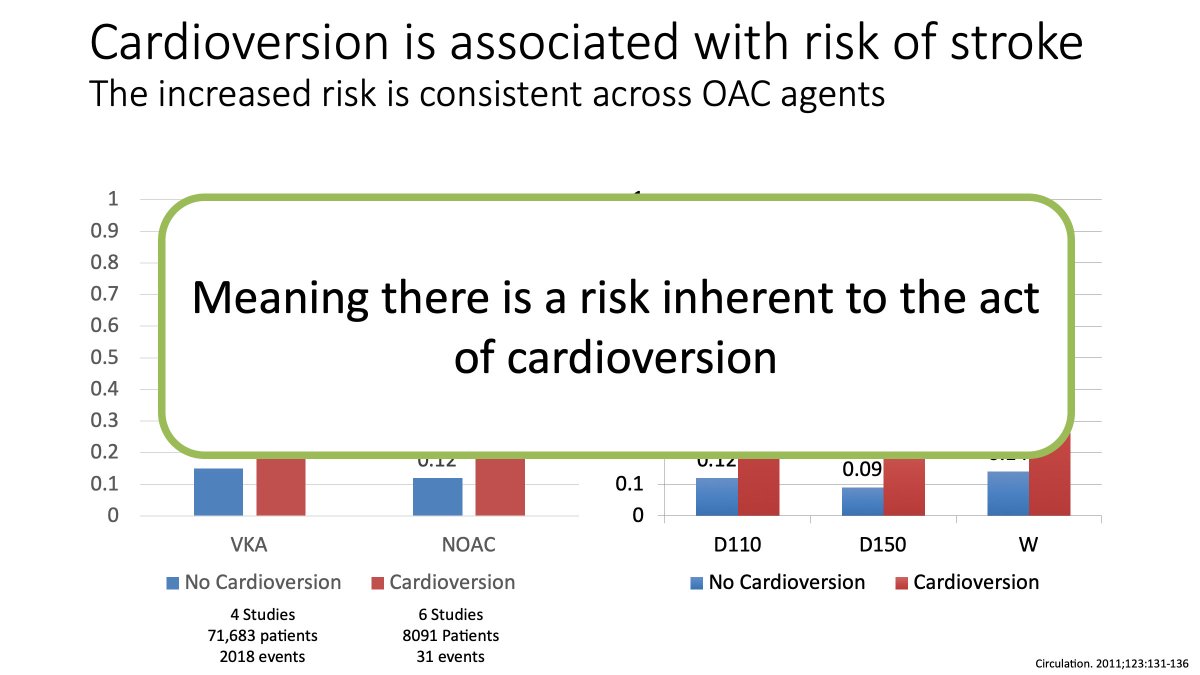
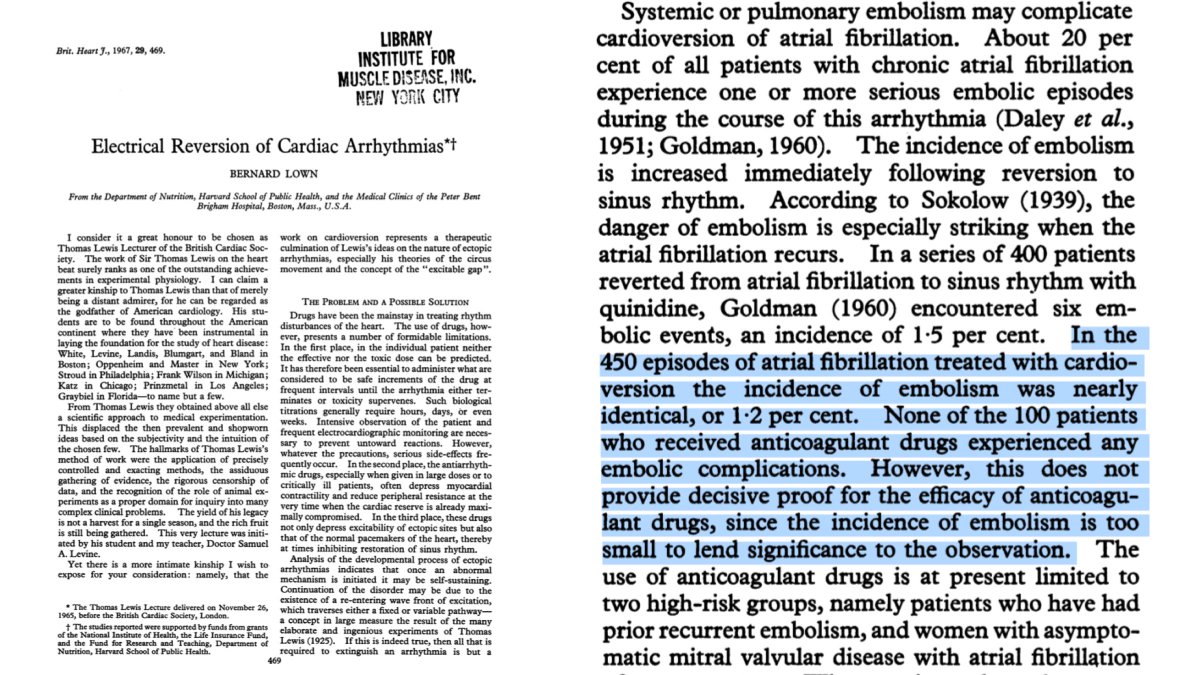
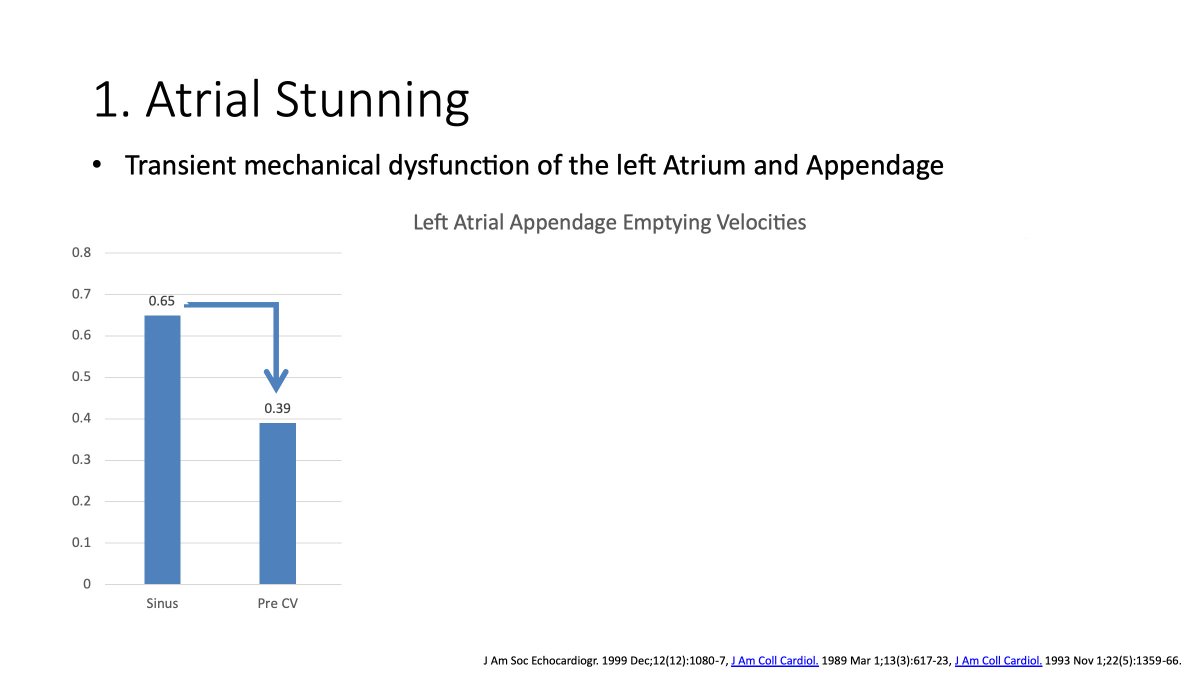
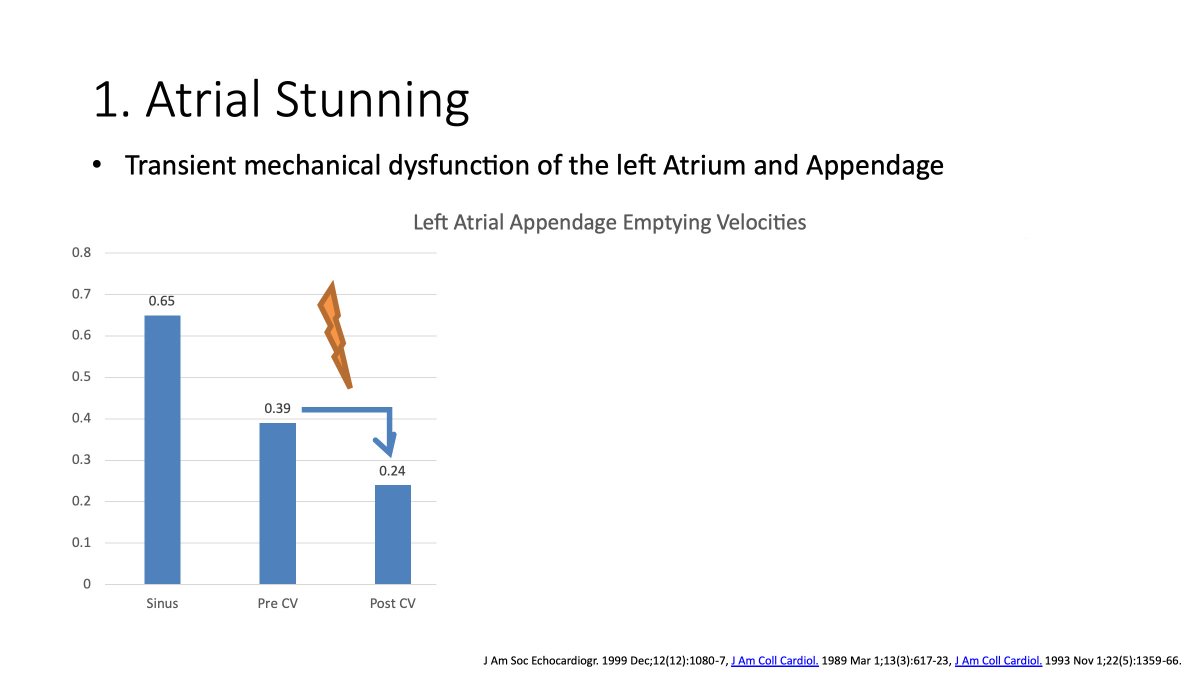
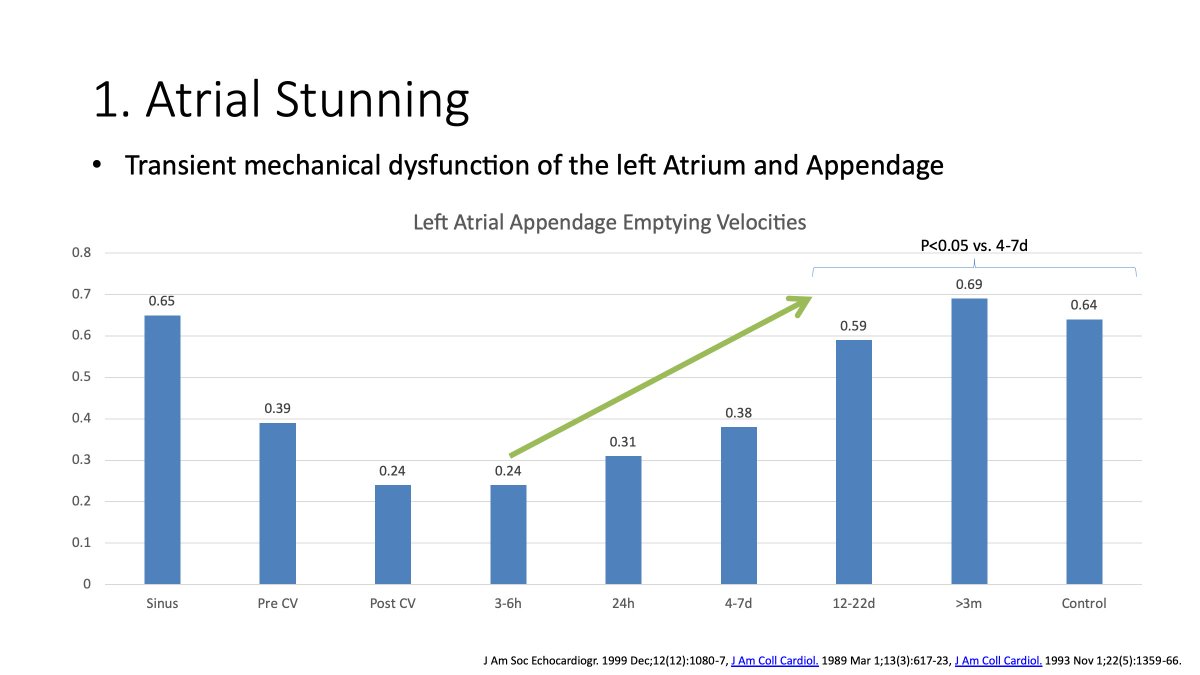
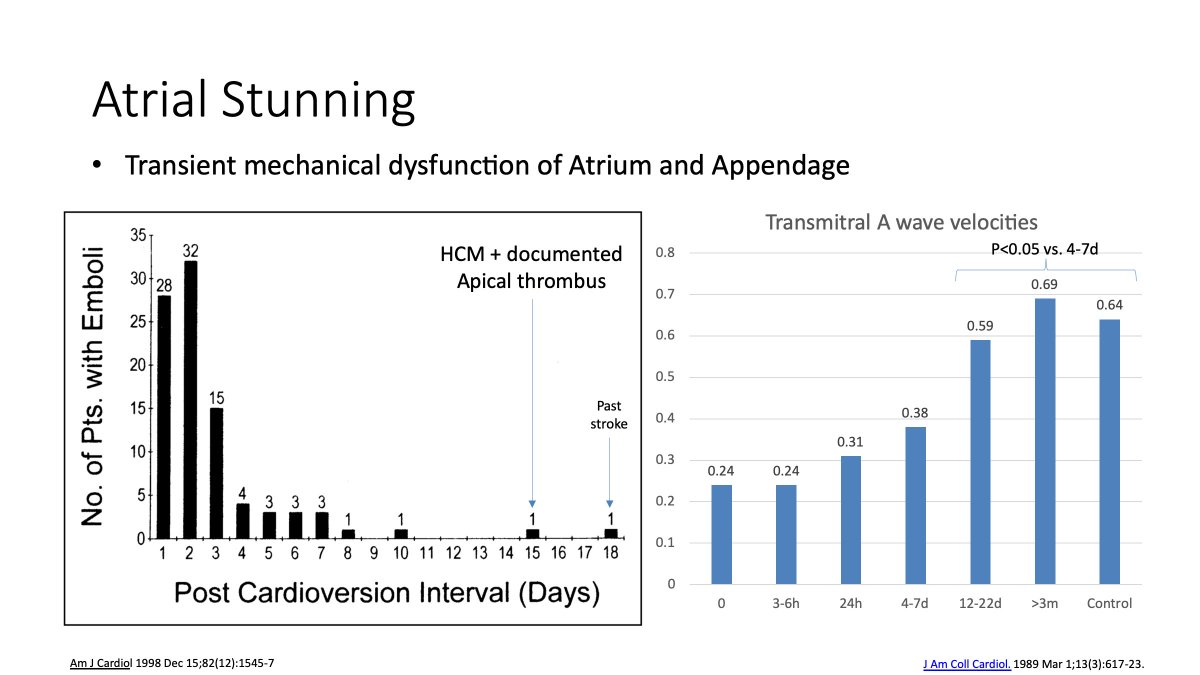
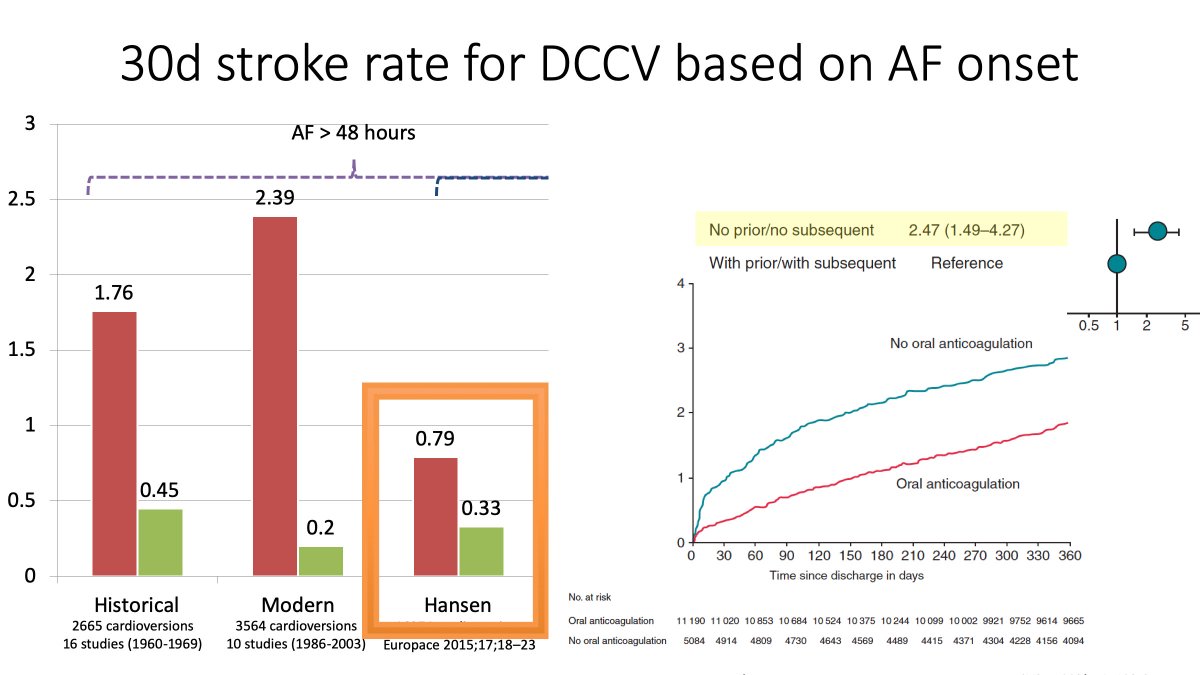
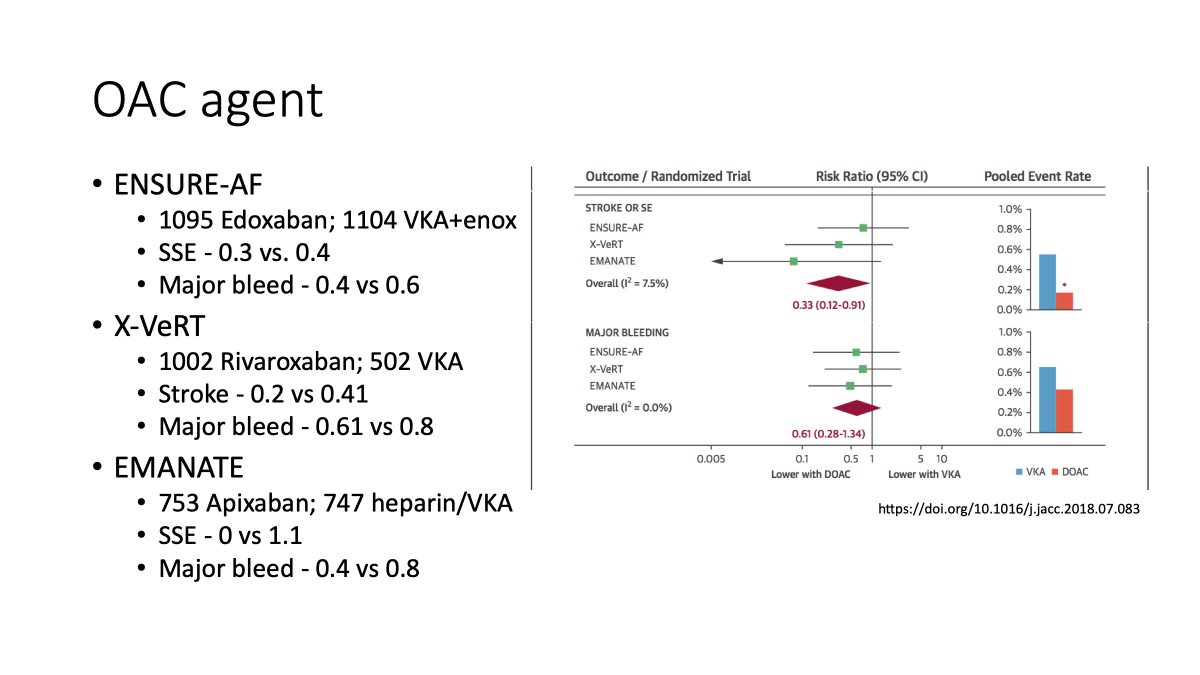
But also recommend OAC for all after pharmacologic or DC cardioversion
More can be found in the following:
onlinecjc.ca/article/S0828-…
onlinecjc.ca/article/S0828-…
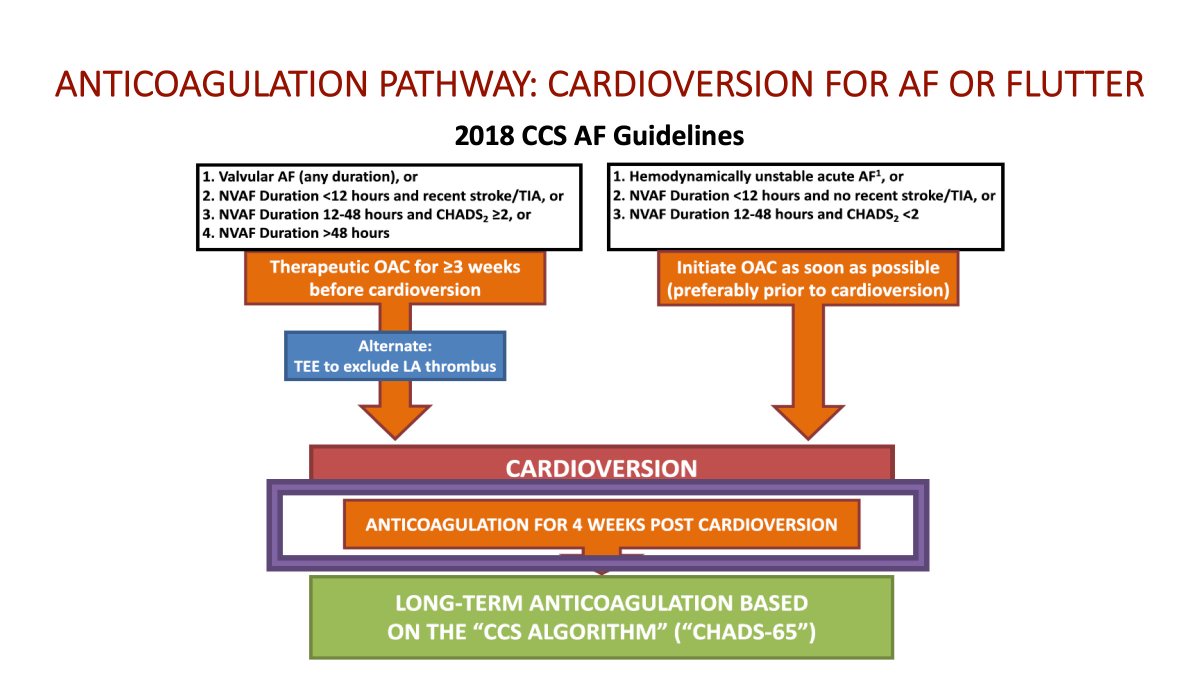
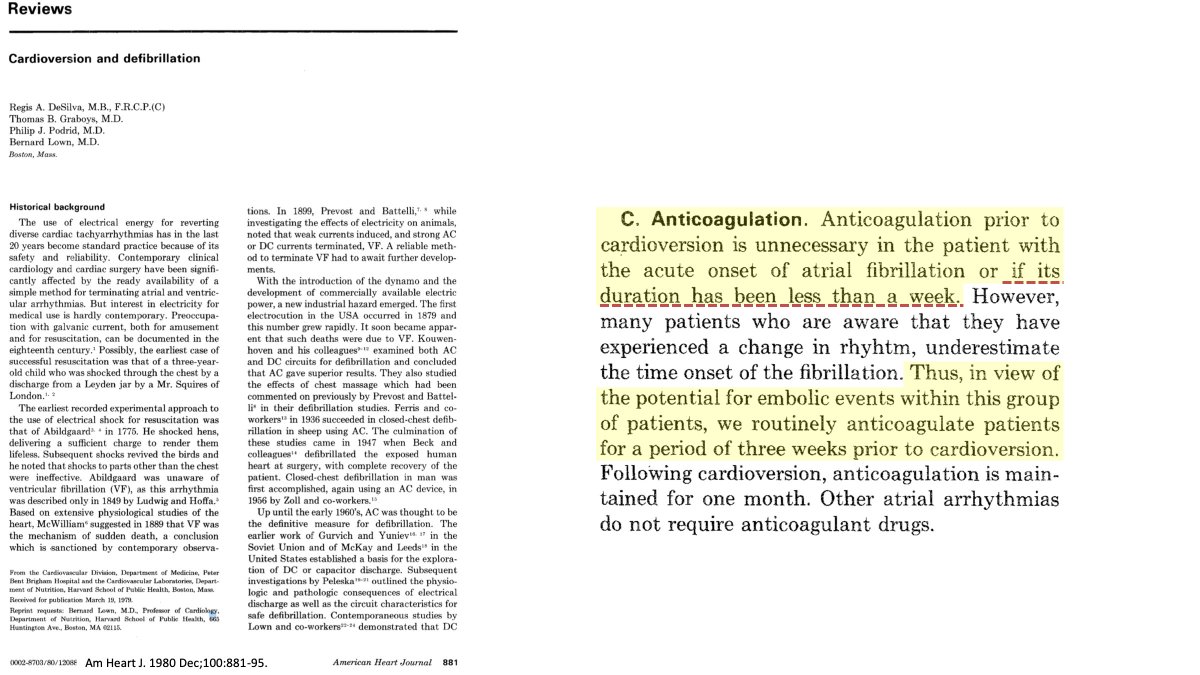
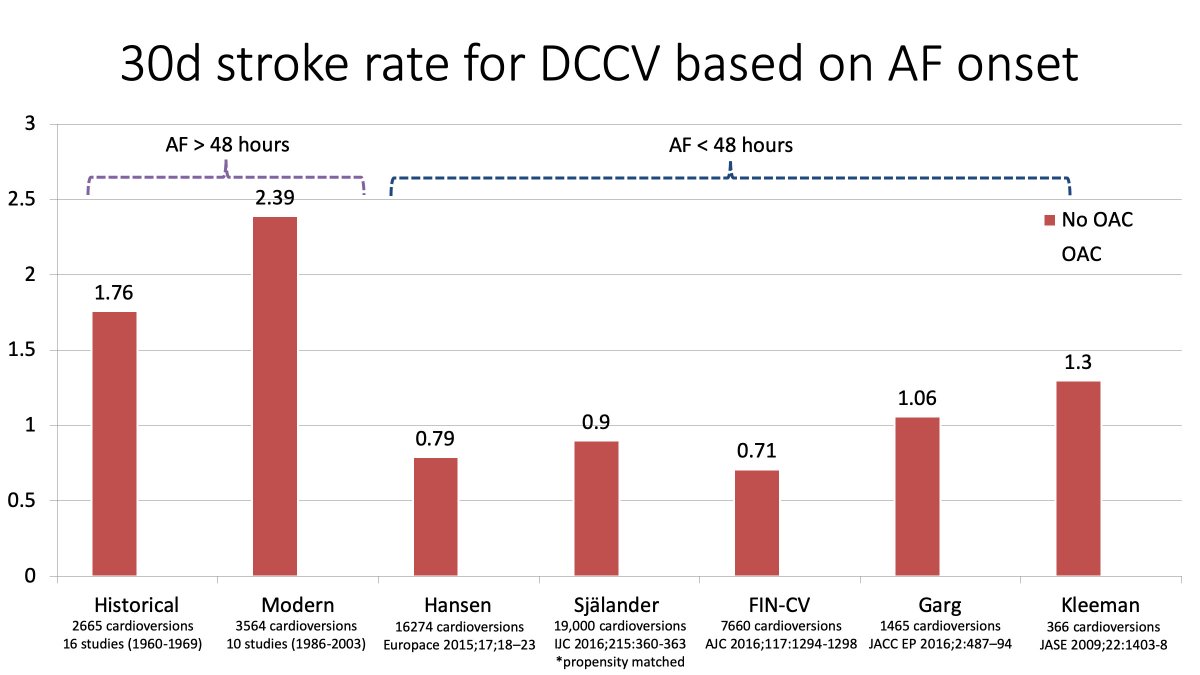
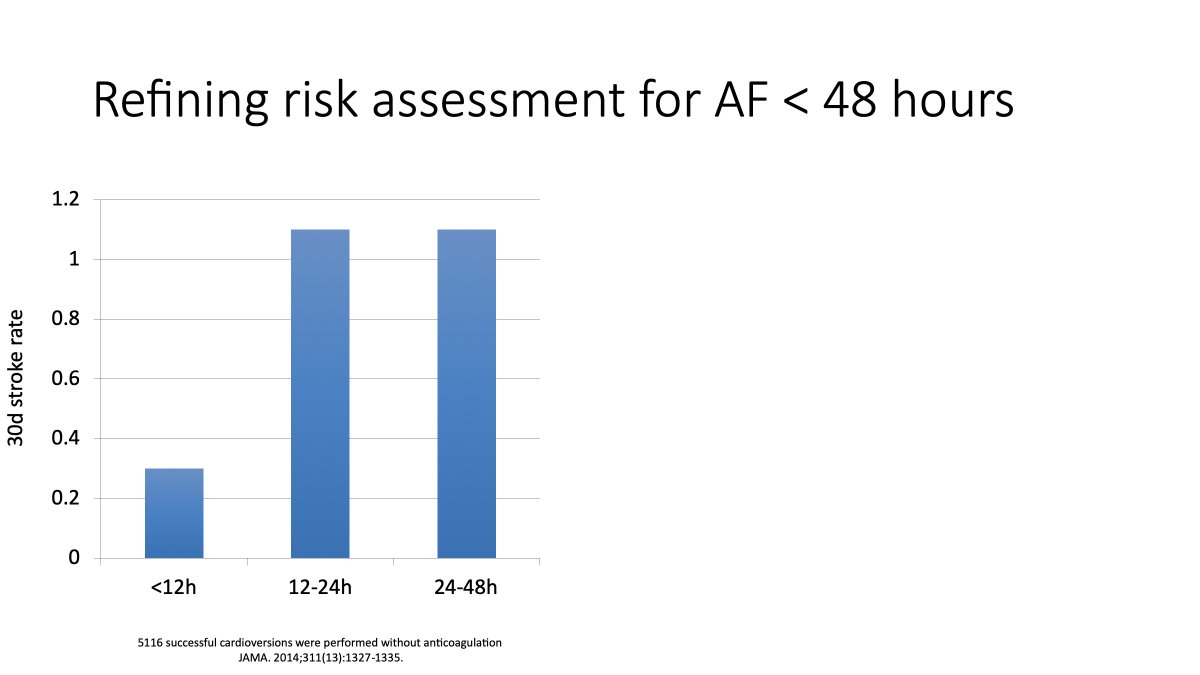
We are more restrictive than most about early cardioversion, suggesting stroke risk be assessed for those presenting between 12-48 hours.
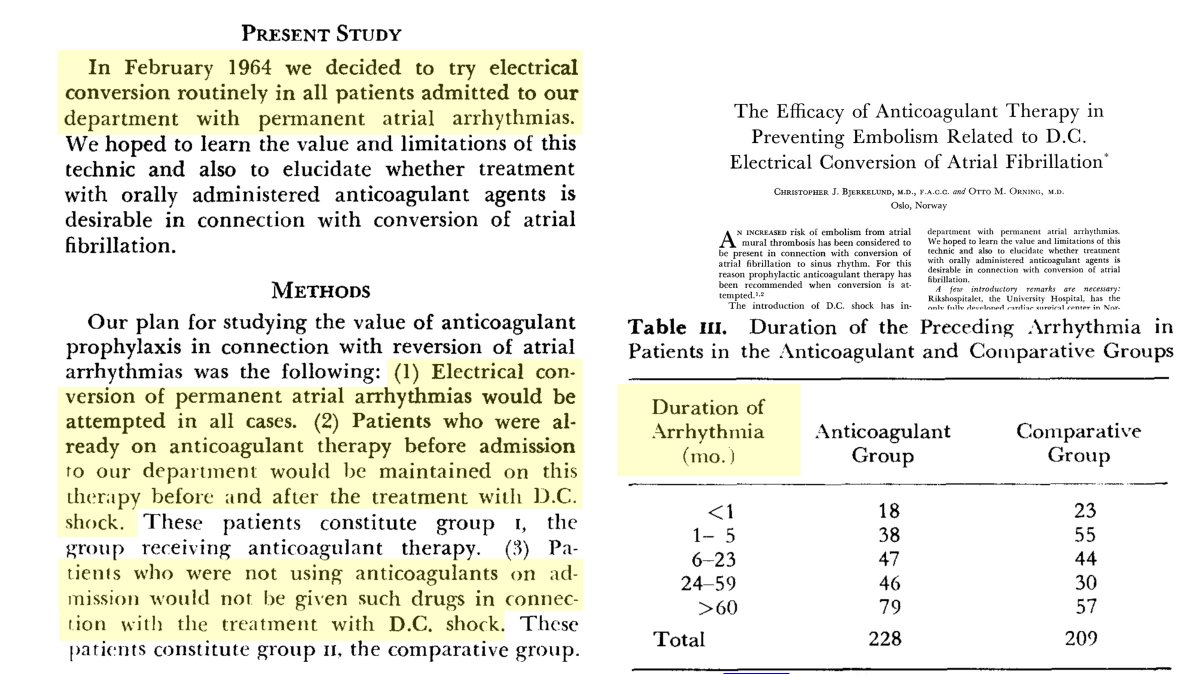
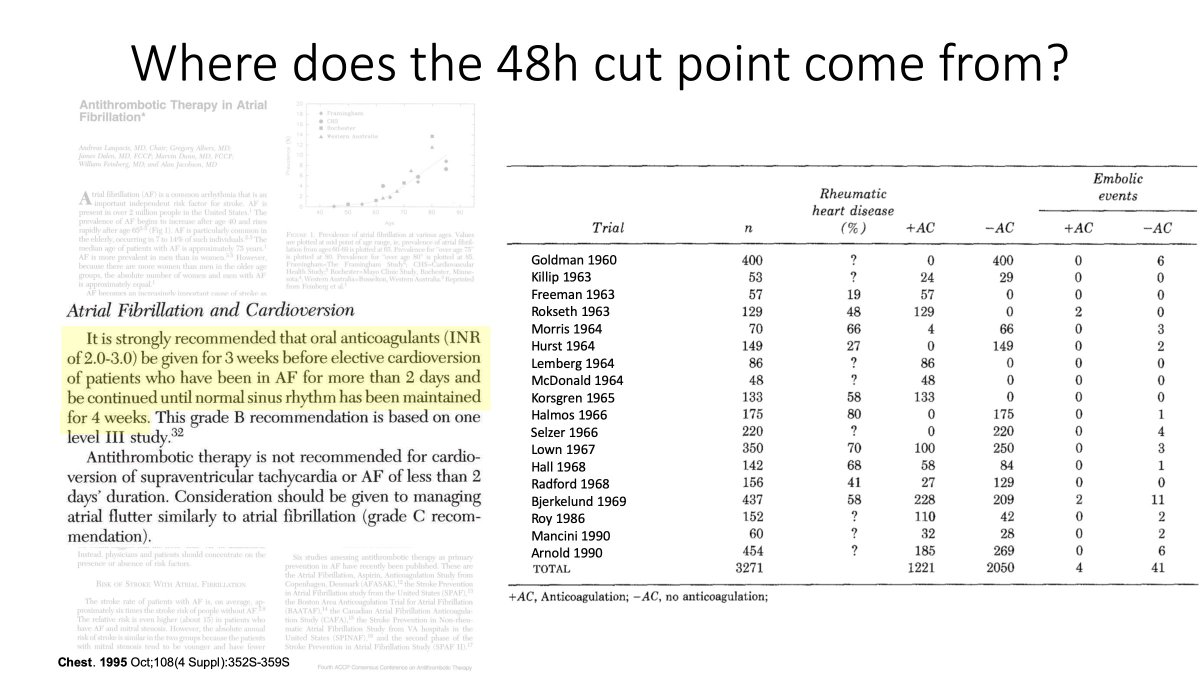
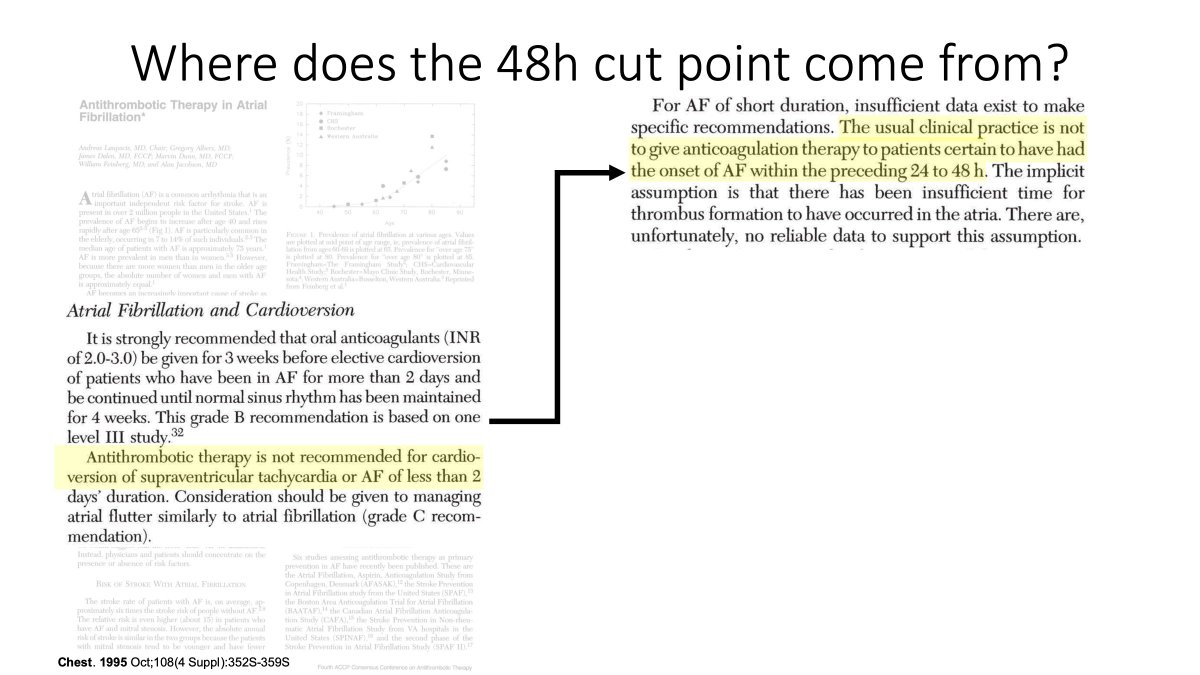
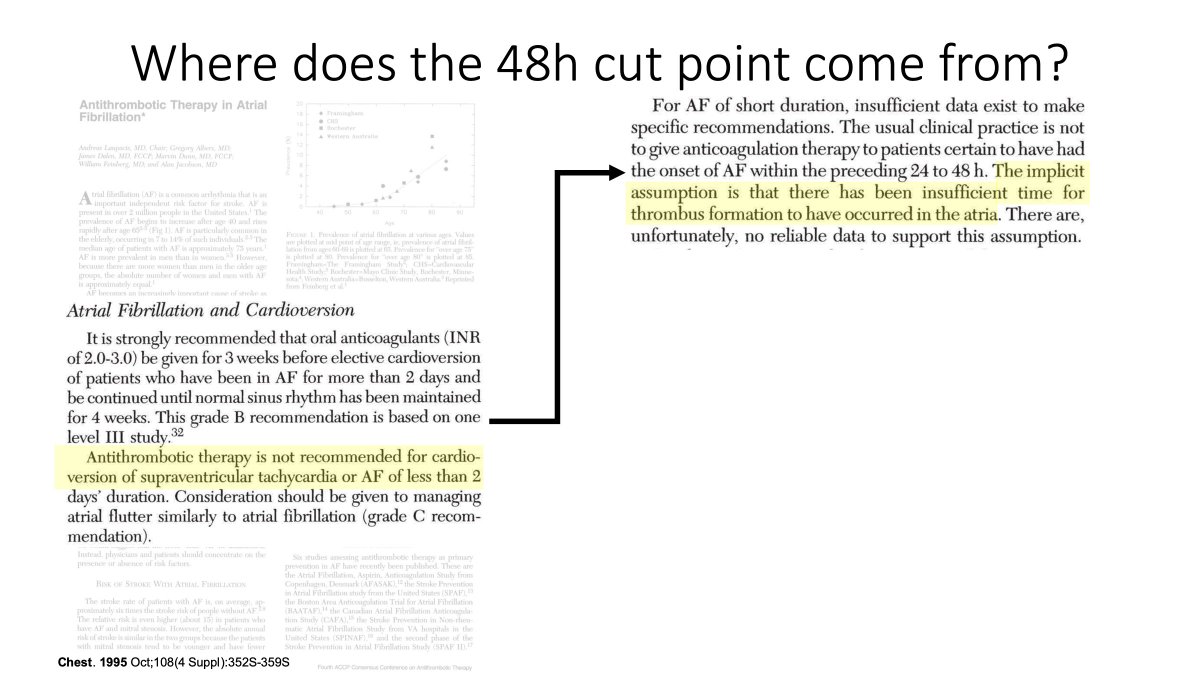
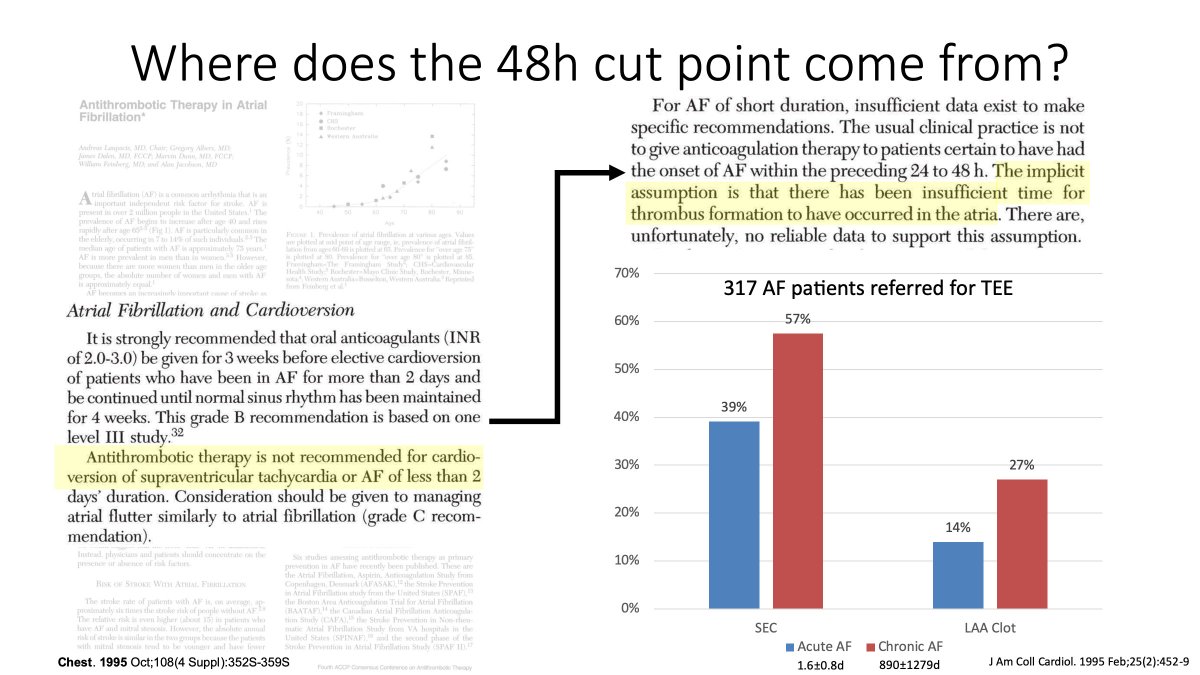
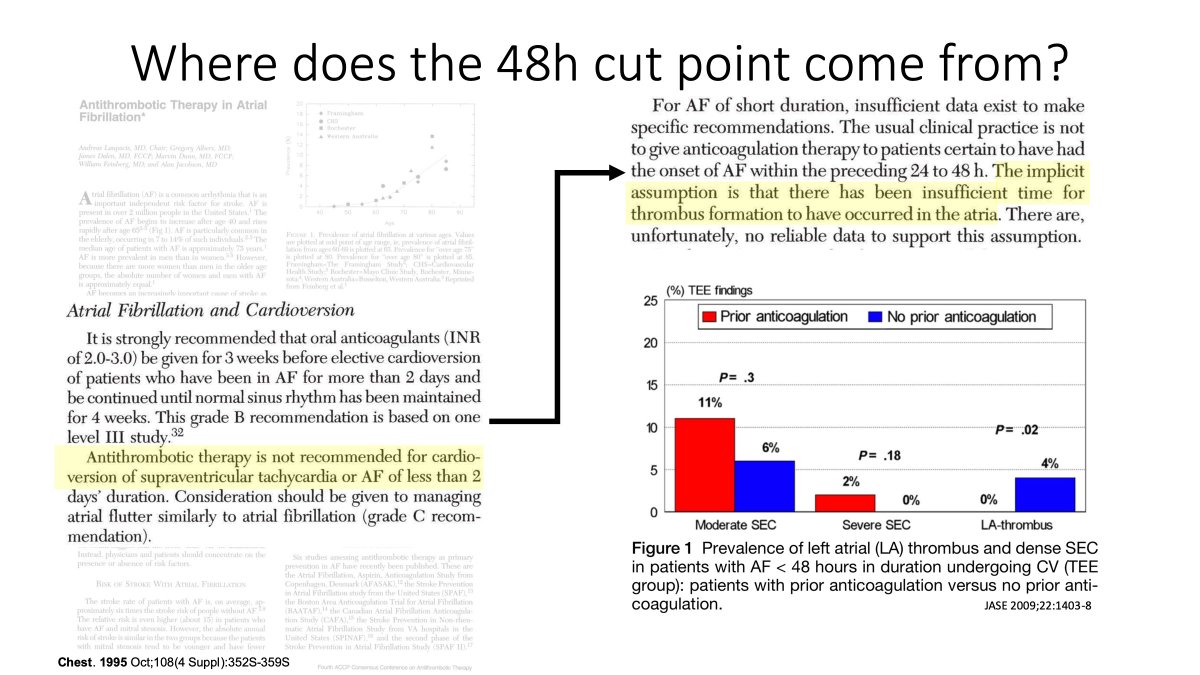
Most other societies would suggest proceeding if AF episode <48h

In this case it is the @ACCinTouch @American_Heart who do not advocate for a period of post cardioversion OAC therapy