blog.cardiogr.am/detecting-atri…
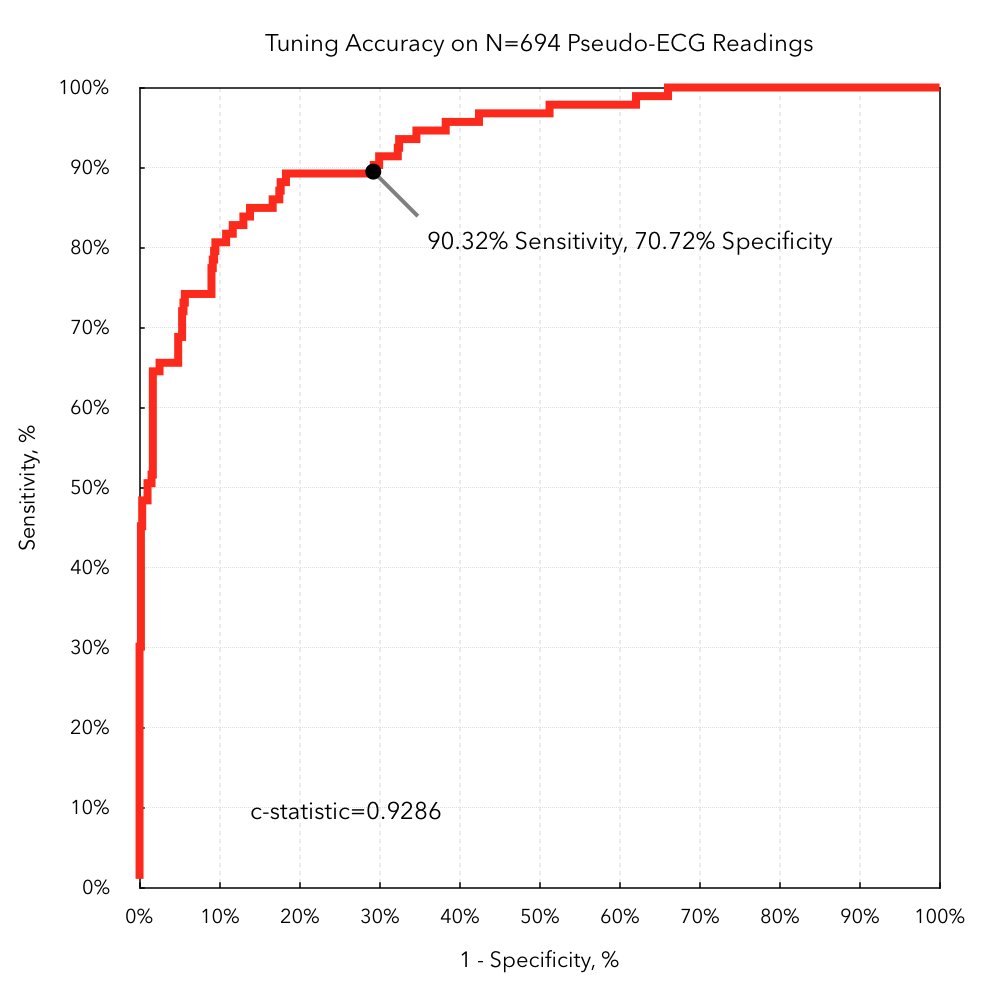
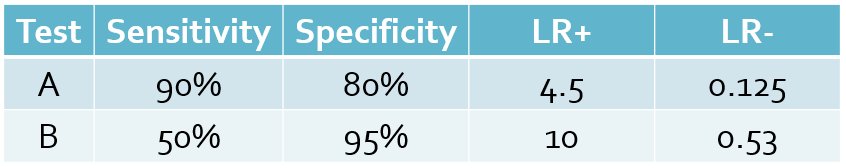
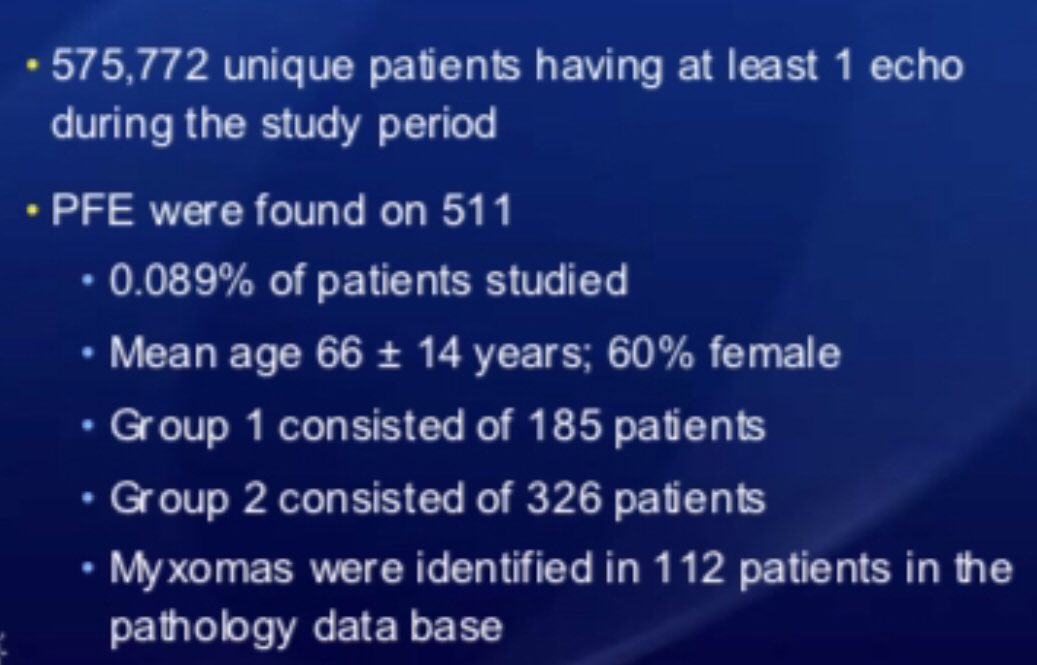
- 90% sensitivity
- 80% specificity
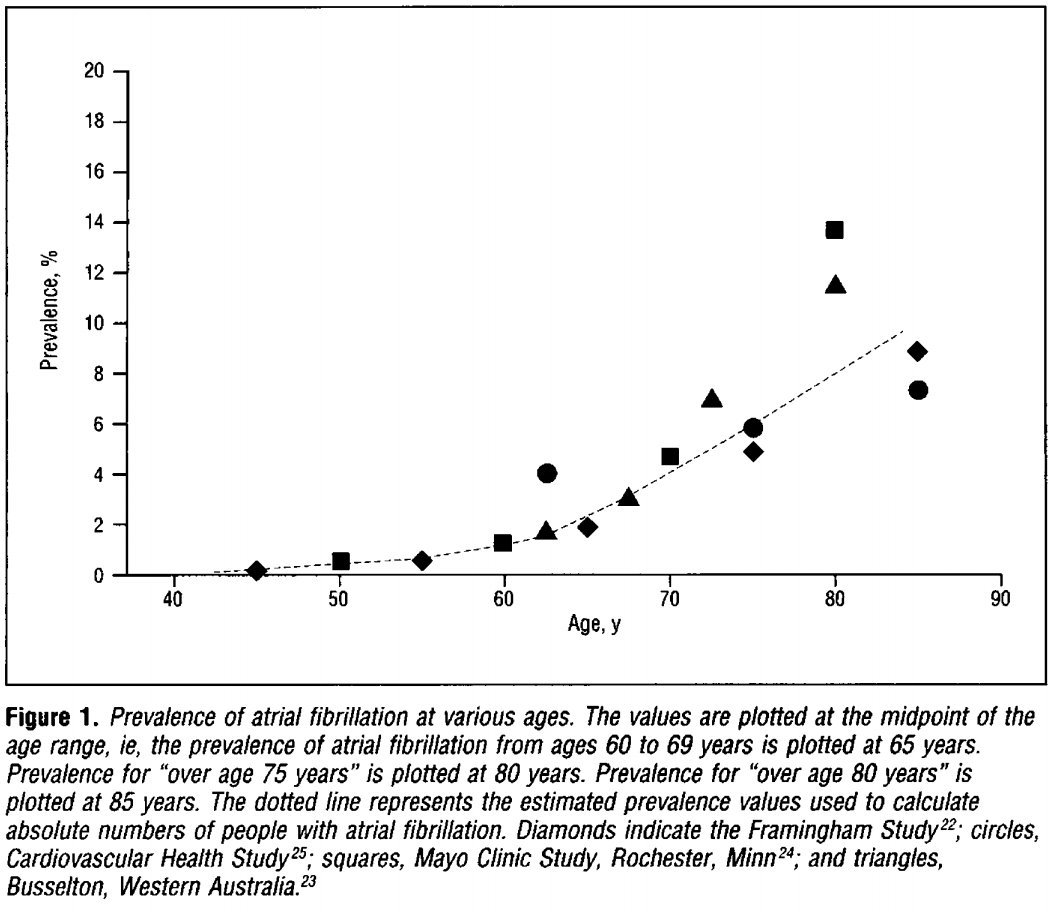
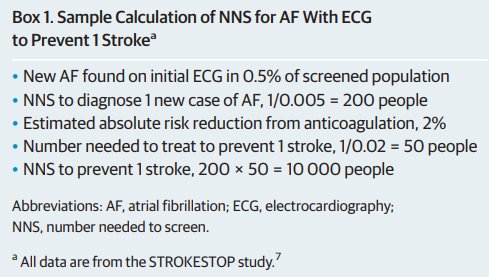
- 0.5% age-based prevalence
Sensitivity = P(Test+ | Disease+)
Specificity = P(Test- | Disease-)
Prevalence = P(Disease+)
Positive Predictive Value = P(Disease+ | Test+)
Negative Predictive Value = P(Disease- | Test-)
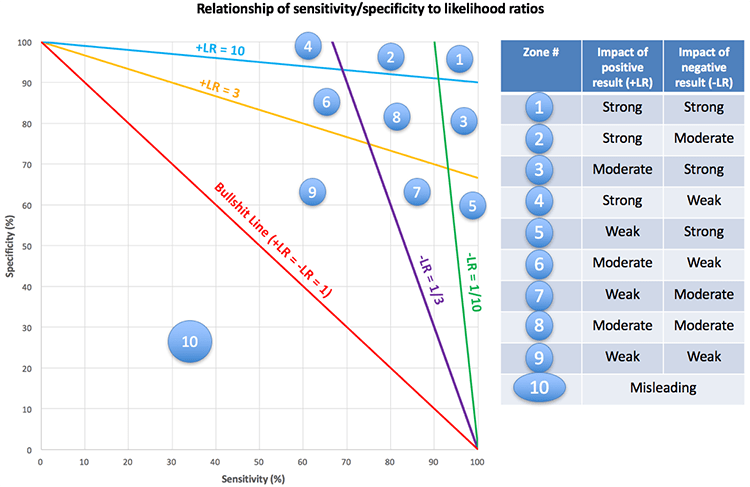
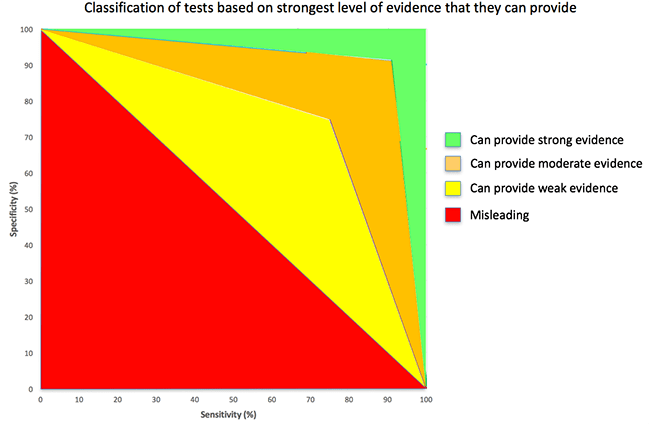
Positive Likelihood Ratio (LR+) = Sensitivity / (1-Specificity)
Negative Likelihood Ratio (LR-) = (1-Sensitivity) / Specificity
Odds Ratio = LR+/LR-
Post-test Odds = Pre-test Odds x Likelihood Ratio
(Use LR+ or LR- depending on test result)
(Can chain together product of multiple LRs)
Post-test Prob = Post-test Odds / (1 + Post-test Odds)
P(Disease+)
--------------
P(Disease-)
P(Disease+) x P(Test+|Disease+)
-------------------------------------
P(Disease-) x P(Test+|Disease-)
P(Disease+|Test+) * P(Test+)
---------------------------------
P(Disease-|Test+) * P(Test+)
en.wikipedia.org/wiki/Bayes%27_…
P(Disease+|Test+)
---------------------
P(Disease-|Test+)
P(Disease+|Test+) = Post-Test Odds / (Post-Test Odds + 1)
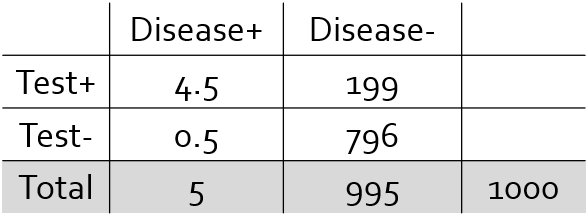
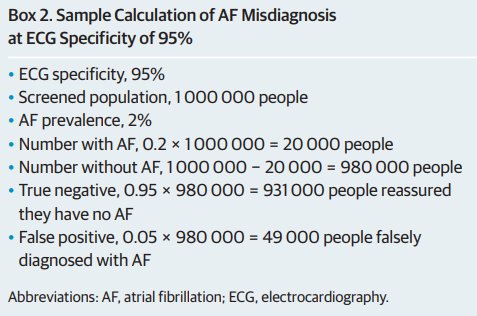
Pre-Test Probability = 0.5%
Pre-Test Odds = 5:995 ~ 0.005
Positive Likelihood Ratio = 0.90/(1-0.80) = 4.5
Post-Test Odds = 0.005 * 4.5 = 0.0225
Post-Test Probability = Positive Predictive Value = 0.0225 / (0.0225+1) ~ 2.2%
Pre-Test Odds ~ 0.005
Positive Likelihood Ratio (Test A) = 0.90/(1-0.80) = 4.5
Negative Likelihood Ratio (Test B) = (1-0.50)/0.95 = 0.53
Post-Test Odds = 0.005 x 4.5 x 0.53 = 0.012
Post-Test Prob = 0.012 / (0.012+1) ~ 1.2%
emcrit.org/pulmcrit/mythb…