In 1948, in what many call the first randomized control trial, streptomycin + bedrest was tested against bedrest alone for the treatment of TB.
Streptomycin treatment led to more radiologic improvement and fewer deaths.
ncbi.nlm.nih.gov/pubmed/18890300
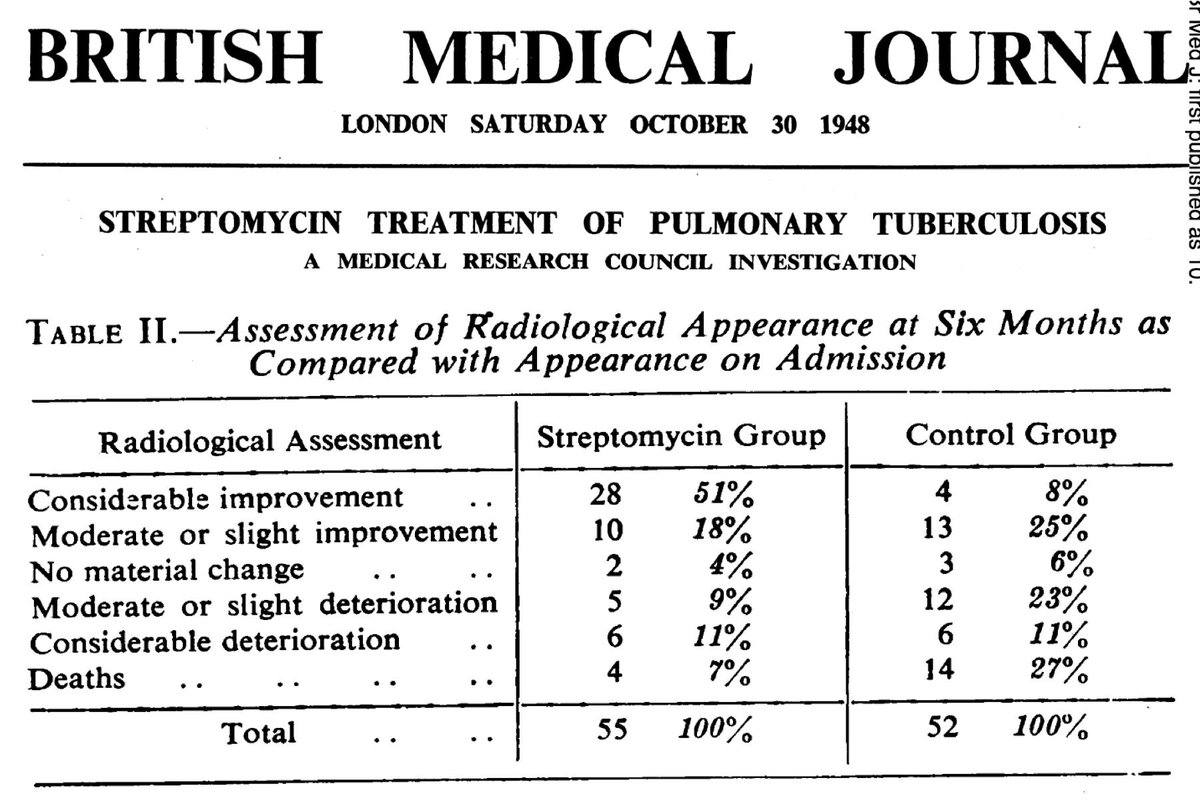
But, there was a problem: 35/41 (85%) of the strains available for testing showed resistance within 6 months.
Which of the following characteristics of TB may contribute to high rates of streptomycin resistance?
[HGT = horizontal gene transfer]
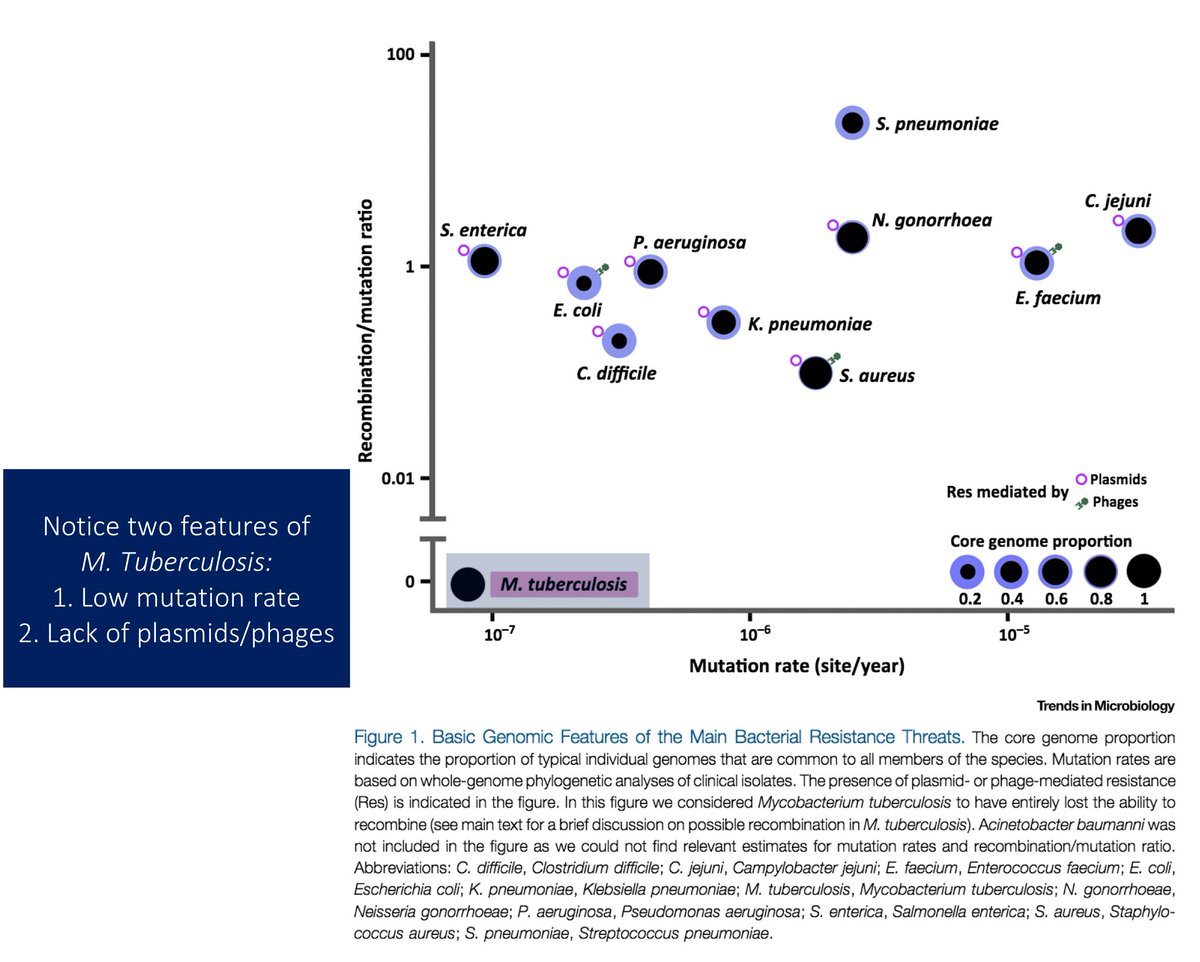
If anything, TB is poorly suited for the acquisition of resistance.
TB:
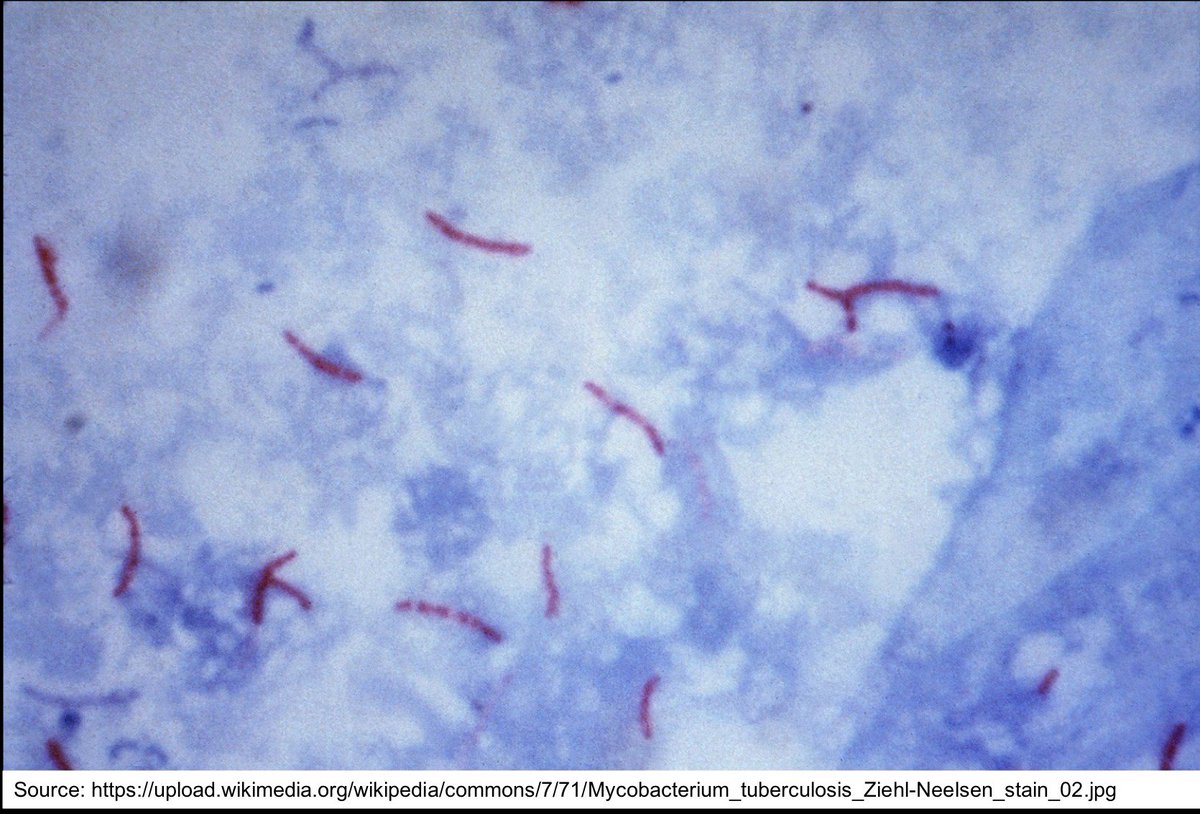
⭐️has a low mutation rate (see Pic)
⭐️has limited genetic diversity
⭐️doesn't engage in horizontal gene transfer
Something else must explain the generation of drug resistance!
ncbi.nlm.nih.gov/pubmed/27068531
Recall that some treatment regimens for latent TB are single-agent. Maybe differences between latent and active TB can provide clues for why the latter requires multi-drug regimens.
Active TB has:
⭐️more cavitary disease
⭐️higher bacterial burden
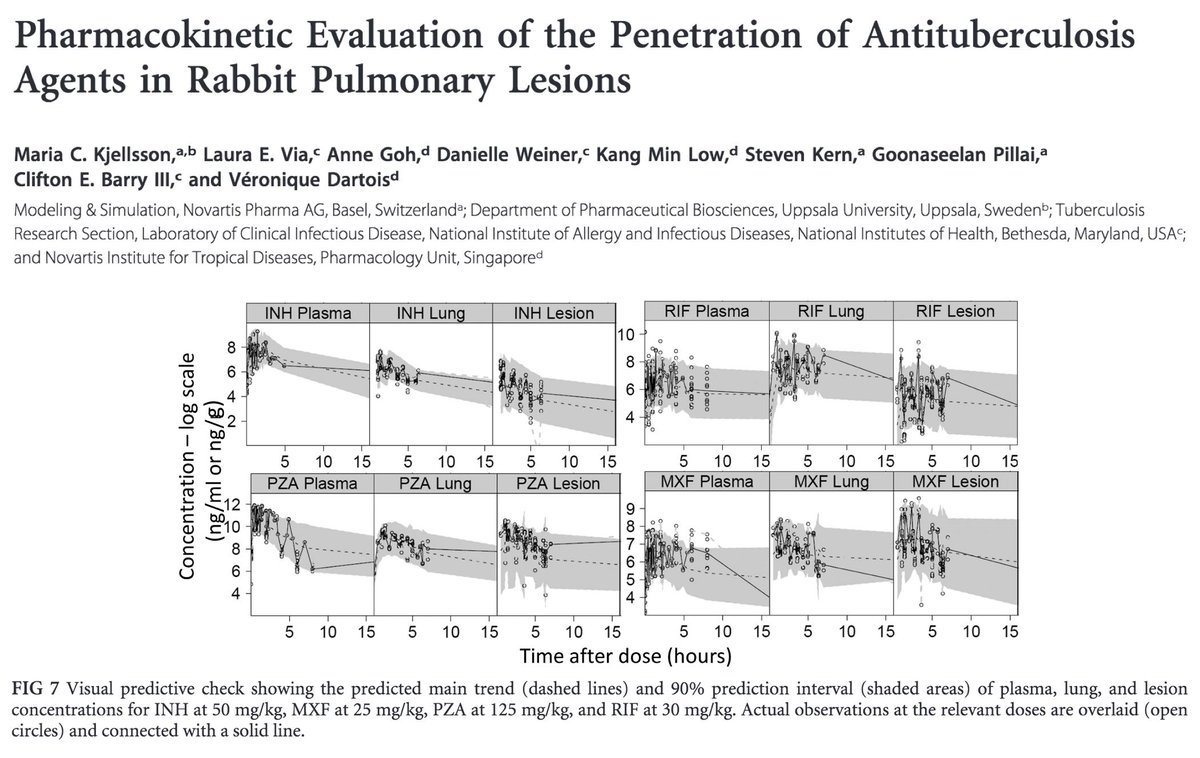
Studies suggest that anti-TB drugs penetrate target tissues to varying degrees (e.g., moxifloxacin >> isoniazid).
Cavities, with their dense, fibrous capsule may not allow for adequate drug penetration, leading to lower local drug concentrations.
ncbi.nlm.nih.gov/pubmed/21986820
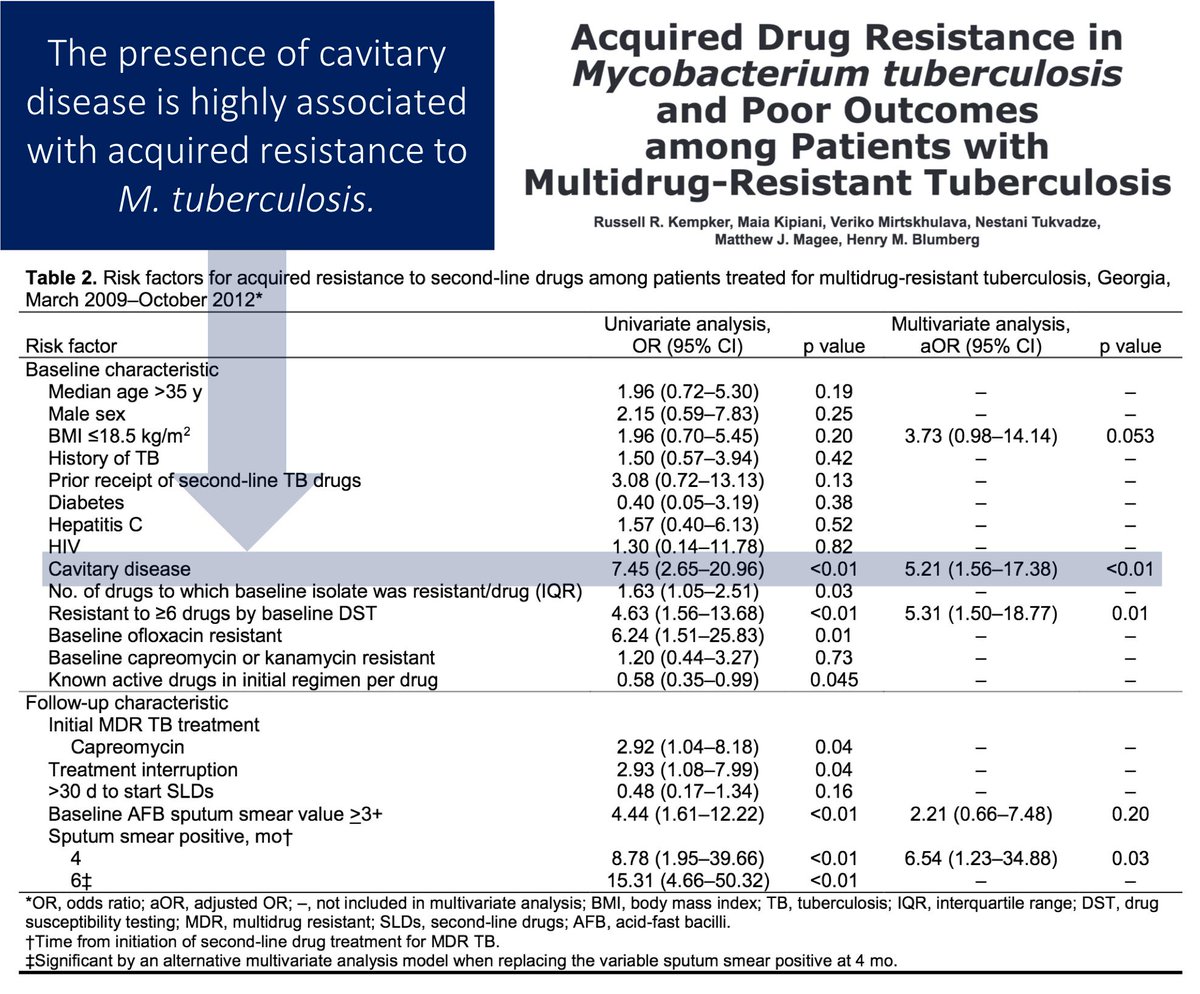
Possibly as a result of the poor penetration into cavities and lower drug concentrations, acquired drug resistance is higher in patients with cavitary disease.
One way to combat this is to give more than one drug.
ncbi.nlm.nih.gov/pubmed/25993036
Cavities also have a LOT of bacilli, at least when compared with what is found in latent TB.
And, bacterial burden is associated with the acquisition of drug resistance.
ncbi.nlm.nih.gov/pubmed/17928422
ncbi.nlm.nih.gov/pubmed/4991927
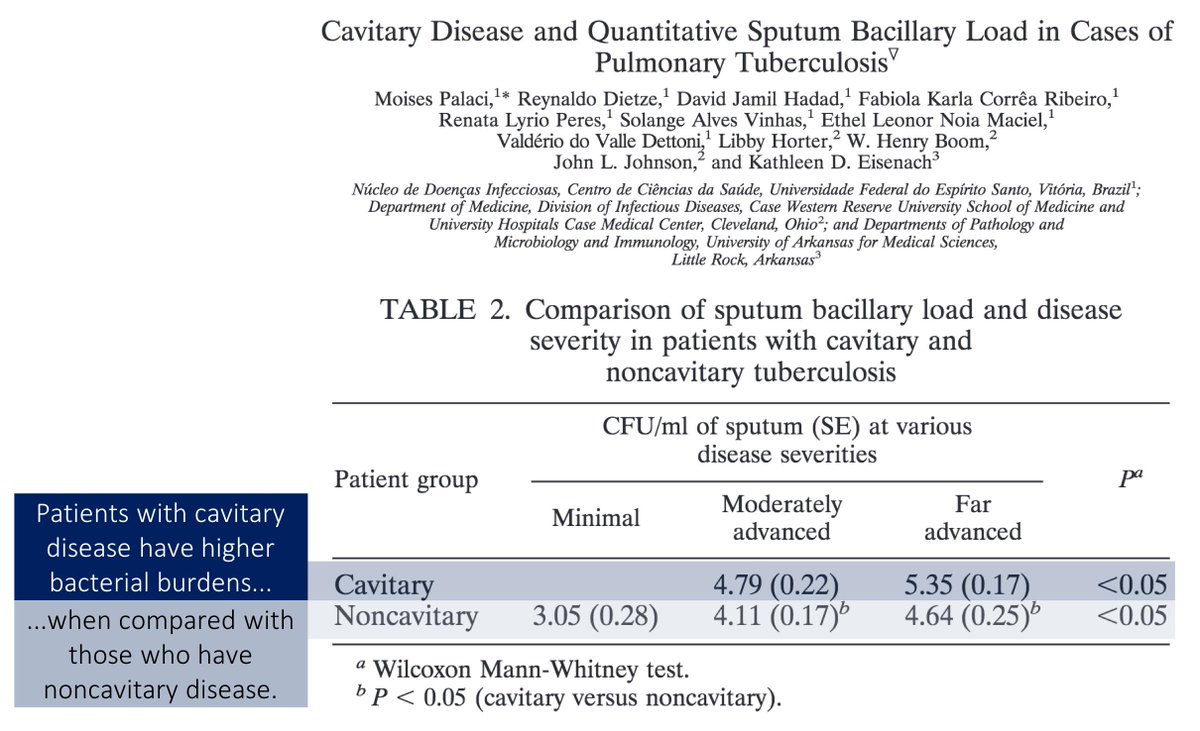
It is estimated that the probability of developing spontaneous resistance to three drugs is around 1 in 10¹⁵, far higher than what is found in cavitary TB (~10⁸ bacilli).
Multi-drug regimens should protect against a mutant bacillus taking over!
ncbi.nlm.nih.gov/pubmed/28292983
✔️Although TB has a low mutation rate, resistance can develop when bacterial load is high and when the bacteria are in poorly penetrated sites.
✔️These are characteristics found more commonly in active TB.
✔️We can overcome this with multi-drug regimens.
Let's explore another issue that is similarly interesting and which also provides insights into why we need multi-drug regimens.
Why do we need to treat TB for months? For other pulmonary infections, we can use as few as 5 days. What's different about M. tuberculosis?
When INH is given, >99% of TB is killed in the first 2 days.
The remaining bacilli are genetically sensitive but phenotypically resistant to INH. And while the MIC for INH is unchanged, it takes months to kill them.
These are "persister cells".
link.springer.com/book/10.1007%2…
To understand what is happening, recall that most antibiotics require bacterial replication to work.
Persister cells are slow growing or non-multiplying bacilli (e.g., they're in the stationary phase). This renders them "phenotypically resistant".
ncbi.nlm.nih.gov/pubmed/17388672
Persister cells are one reason that TB requires months of treatment.
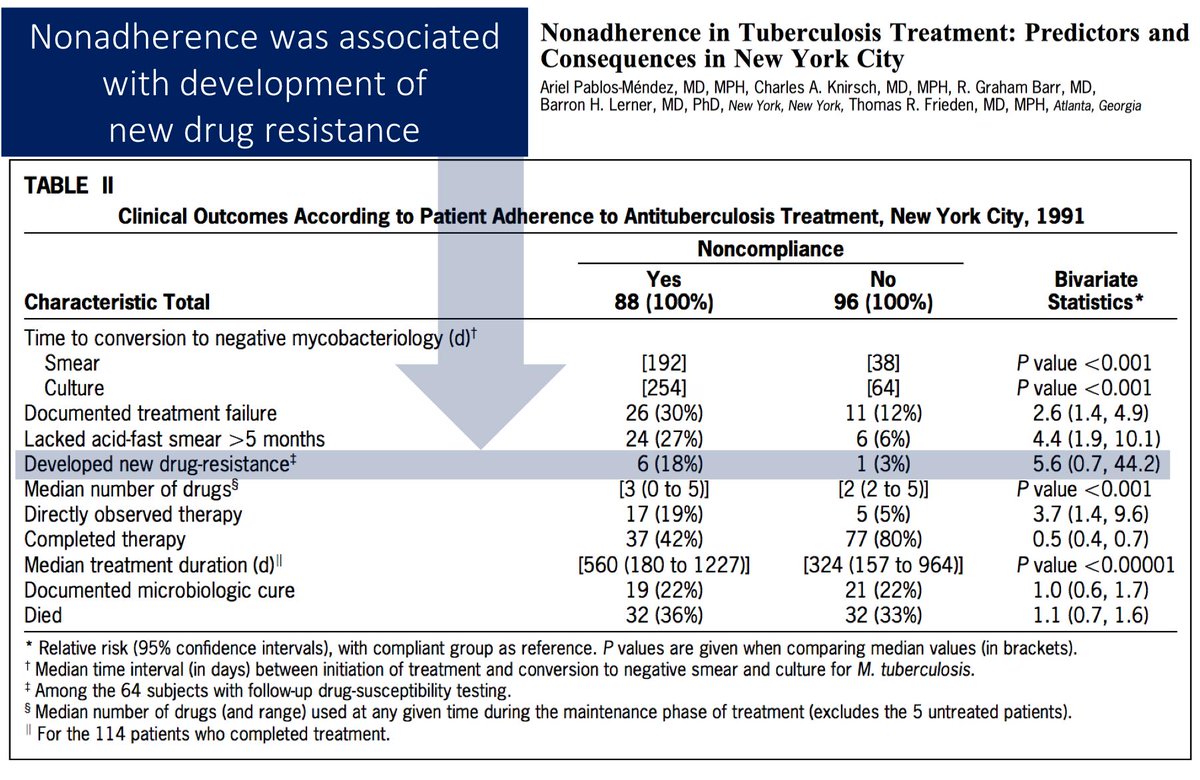
Unfortunately, with months of treatment comes many opportunities for missed doses. This may also contribute to the acquisition of drug resistance.
ncbi.nlm.nih.gov/pubmed/9217566
Before summarizing, let me ask a closing question.
Which of the following partly explains why we use multiple drugs to treat active tuberculosis?
✔️Despite a low mutation rate, TB generates resistance to antibiotics within months of monotherapy
✔️Presence of cavitary disease and high bacterial burdens play a role
✔️Persister cells necessitate months of therapy; this may contribute via incomplete adherence