This salty #tweetorial will pose some questions and explore common pitfalls of using IV fluids “for maintenance.”
If someone is volume down, give them a bolus.
“Maintenance fluids” are often the wrong choice because they’re not enough.
What’s the harm in a little extra IV fluid, you say? Let’s do some easy math.
Isotonic fluids
- Normal saline: 154 mEq Na, 154 Cl
- Lactated ringers: 130 Na, 110 Cl, 28 lactate, some K and Ca
Hypotonic fluids
- Half/quarter NS: divide above by 2 or 4
- D5W: 50g dextrose (200 calories) per L
Can add dextrose or K to any fluid.
100cc/hr NS = 2.4 L/day = 22 grams of IV salt per day. After day. After day.
Few hearts/kidneys are healthy enough to handle that.
bit.ly/2XFF7AR
bit.ly/2XL1akV
Yep. But as far as salt load and potential for overload, LR is about the same.
Me neither.
We’re all NPO after midnight. Being NPO overnight isn’t a reason to start someone in IV fluids.
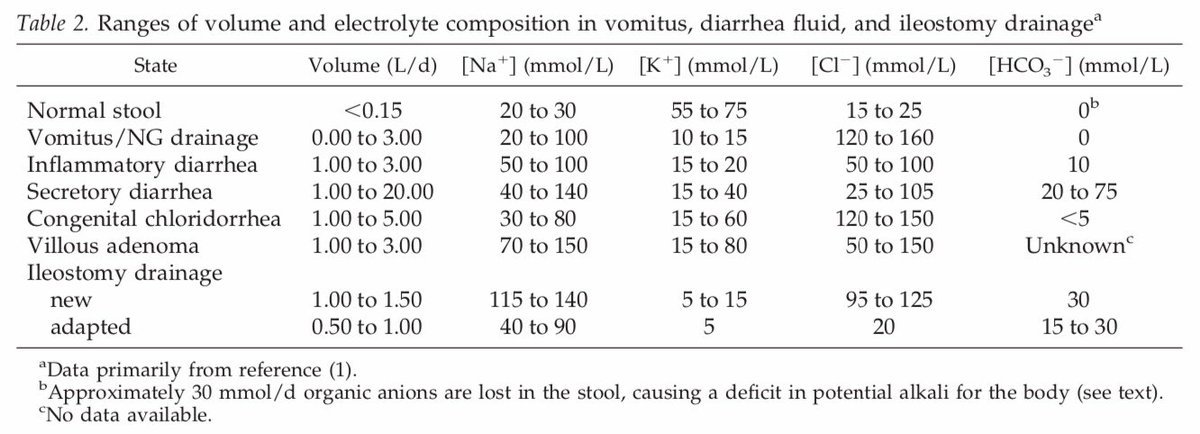
Breath caries free water
Sweat is ~1/4 normal
Staying alive does cost calories
bit.ly/2YTsj6q
So if it’s those losses we’re maintaining, 1-2L per day of D5-1/4NS or D5–1/2NS +/- some K makes most sense.
bit.ly/30wMxU4
Lady with pyelo, temp 102, WBC 20. Got abx and 2.5 LR in ED, BP recovered, pulse too, 110 -> 70s. JVP, lung exam normal. She’s eating drinking fine.
What fluids do you order now:
Nothing: “Looks like we’ve resuscitated enough, why give more? I’ll reassess soon and if HR/BP drift again, I’ll bolus”
LR: “There’s no way she’s done third-spacing. Let’s keep up.” Key here is best-guessing a finite volume.
Individualize.
- If someone is volume down, bolus LR
- We overuse maintenance fluids and cause lots of iatrogenic HF / volume OD. Be thoughtful about whether indicated.
- If indicated (eg NPO for days), D5-1/2NS @ 75cc/hr may be best default to match hypotonic insensible losses