Why healthcare is incapable of reducing its own costs:
A tutorial system analysis
#M4A #UHC #healthcare #healthcarecosts @ASlavitt @boltyboy #futurist imaginewhatif.com #healthcaredebate #healthforall
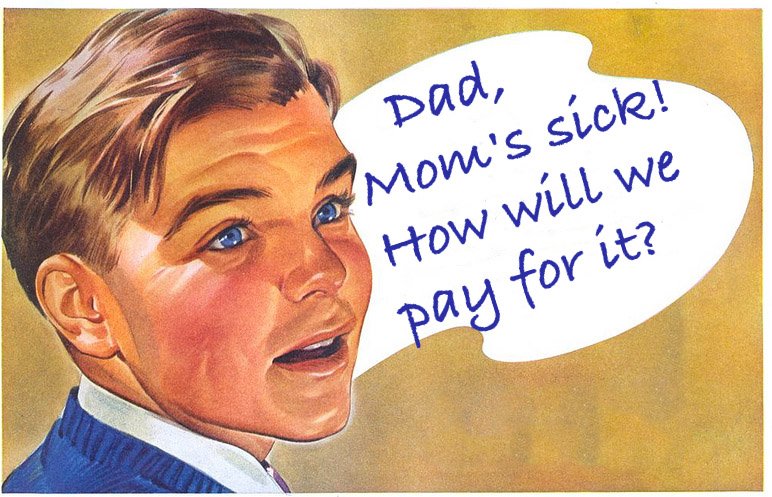
The health insurance industry's hired guns cry that Medicare For All (or any universal healthcare) would "crash the system" and "destroy healthcare as we know it."
They say that like it's a bad thing.
They say we should trust them and their cost-cutting efforts to bring all Americans more affordable health care.
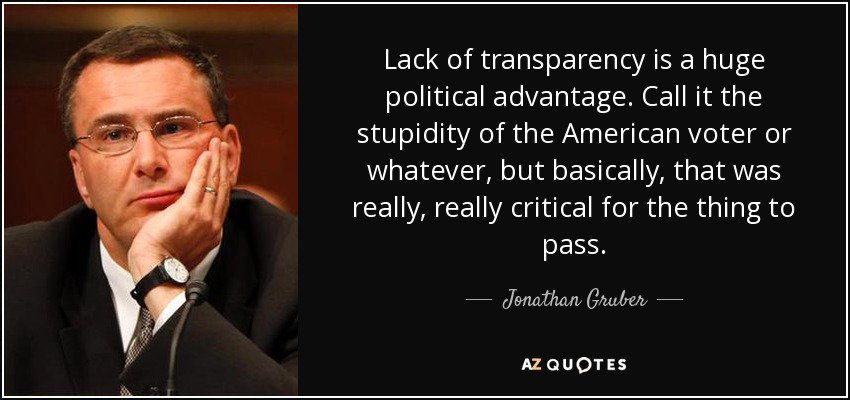
We should not trust them, because the system as it is currently structured economically is incapable of reducing costs.
Why?
Let's do a quick structural analysis.
This is how health care actually works.
Health care, in the neatly packaged phrase of @nicksoman Nick Soman, CEO of @decent Decent.com, is a “system designed to create reimbursable events.”
They have no incentive to reduce the total cost,
and every incentive to increase it.
The ideal customer is the middle of the market, the stable customers, the not-so-sick-or-expensive customers.
So health care providers have largely avoided opportunities to take on risk, to be transparent about their costs, or to guarantee their patients anything at all.
Change can be expensive, difficult, and requires strong leadership.
This combination of consolidation and lack of transparency means that there is no real competition on price and quality among health care providers.
There is no competitive market in health care.
How does this reform plan change the way we pay for healthcare, the economic foundation of the industry?