#medtwitter is fairly comfortable managing “normal” DKA right? But how about in the anuric dialysis patient? The cookbook protocol can be deadly.
Read this #tweetorial to learn about how their DKA pathophysiology is fascinatingly different.
#meded #nephpearls #endotwitter
Recap of normal DKA;
✅ patient symptomatic,extracellularly dry, 6 litres down & counting
✅ whole body K low due to osmotic diuresis, but often ⬆️K at first due to hypertonicity/ low insulin/ acidosis
- serum K then rapidly falls as INsulin drives K & glucose INtracellularly
Usual life-saving protocol involves treating any underlying precipitant, giving iv insulin (& usual subcut insulin) and aggressively repleting volume & electrolytes.
☠️ many protocols don’t mention that for dialysis patients this cookbook medicine can be lethal ☠️
Patients with ⬇️GFR are actually relatively protected from DKA;
👍 decreased exogenous insulin metabolism by kidney proximal tubules = harder to be deficient
👍 in-centre haemodialysis patients seen 3 times a week = earlier illness recognition (despite being less symptomatic)
But dialysis patients do sometimes go into DKA, & are at ⬆️risk of;
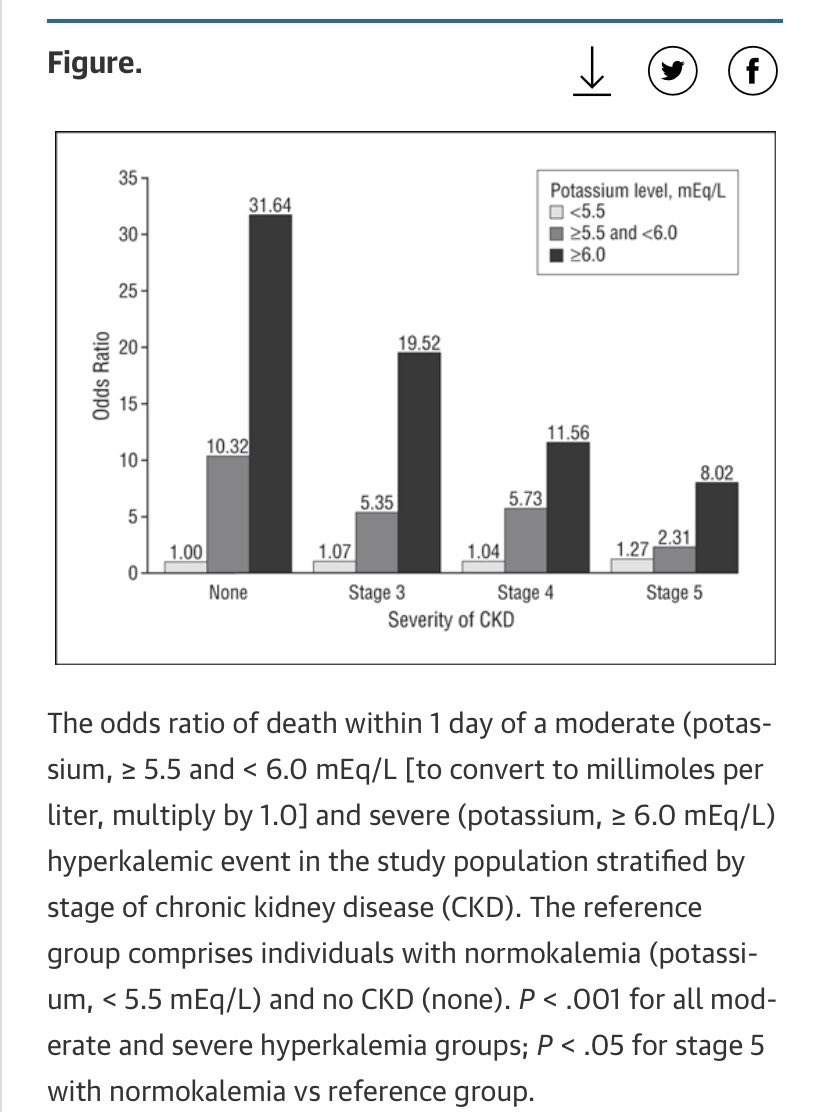
❗️severe hyperkalaemia (limited K excretion)
❗️serious underlying drivers (big two here are ischaemia & infection)
❗️rapid fall in glucose with treatment = higher risk of hypoglycaemia and large tonicity swing
However the key difference in chronically anuric dialysis patient in DKA is...
🔴 no huge osmotic diuresis 🔴
Therefore;
✅ higher initial serum glucose level (as no glycosuria)
✅ removes need for large volume & electrolyte resuscitation
⚠️ hence not for ‘the protocol’ ⚠️
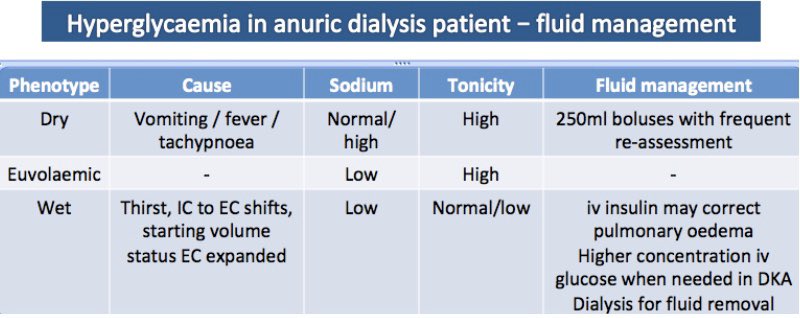
Tzamaloukas 2008 proposed 3 anuric hyperglycaemia phenotypes to help frame managing volume status
1. Dry anuric patient
- due to ⬆️RR/fever/vomiting
- high tonicity, normal/high Na
👉 Mx includes 250ml boluses
2. Euvolaemia
- high tonicity, low Na
👉 Fixes with iv insulin
❗️This is a rather unusual type of pulmonary oedema - it is reversible with iv insulin alone ❗️
(when insulin drives glucose into cells water follows from interstitium = less extracellular water = resolution of pulmonary oedema)
Its well reported that hyperglycaemia causes pulmonary oedema in dialysis patients via these mechanisms even in absence of pre-existing heart disease
This may be even more likely in DKA state due to;
☑️ altered pulmonary capillary permeability
☑️ acute myocardial dysfunction
Other facts about the wet patient in phenotype 3;
👉 Normal initial tonicity provides (insensitive) indirect indication of high fluid consumption in anuric hyperglycaemia.
👉 severity increases with higher initial glucose levels & if volume state uncontrolled to begin with.
Treatment recommendations for DKA in dialysis cohort are based on case reports;
✅ iv insulin
✅ critical care level monitoring of electrolytes, glucose & volume state
✅ be aware of ⬆️hypo risk (especially associated with insulin bolus in case series)
✅ say no to iv bicarb
Treatment (cont)
✅ small fluid boluses with re-assessment if hypovolaemic
✅ if hypervolaemic, go with higher concentrations of iv glucose when the sugars fall
✅ caution with K replacement
✅ high index suspicion for infective / ischaemic precipitants
Big obvious question is; given the anuric patient in DKA is often hyperkalaemic, volume overloaded & acidotic - doesn’t dialysis just fix all those things?
As you’d expect there’s no good evidence on potential harms, or whether early or late dialysis strategy best.
Clearly if hyperK or volume overload is life-threatening then easier decision.
Potential downsides to early HD;
❌ doesn’t fix underlying pathophysiology of insulin deficiency (if anything dialyse out insulin)
❌ masks severity
❌ cerebral oedema risk from tonicity swing
Key learning points aren’t anything about anuric DKA - you may never see this.
It’s that the rules are always different in dialysis patients. Treatments are less tried and tested. Evidence base = case reports. Familiar protocols can become dangerous. Call for help early.
As ever, I’m a trainee so any disagreements / criticism / sharing experience much appreciated.
References;
sciencedirect.com/science/articl…
ncbi.nlm.nih.gov/m/pubmed/67652…
cambridge.org/core/services/…
ncbi.nlm.nih.gov/pmc/articles/P…
ncbi.nlm.nih.gov/pmc/articles/P…