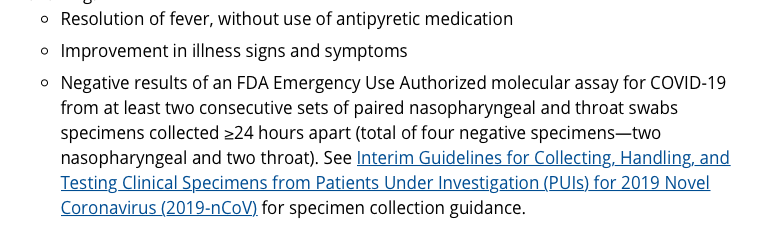
May be removed from transmission-based precautions on a case by case basis (neg pressure rooms, PPE etc).
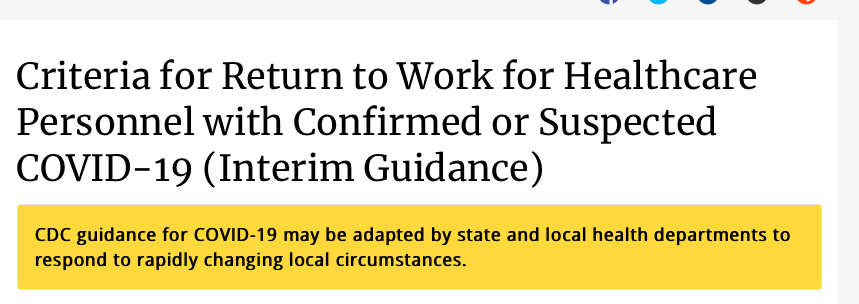
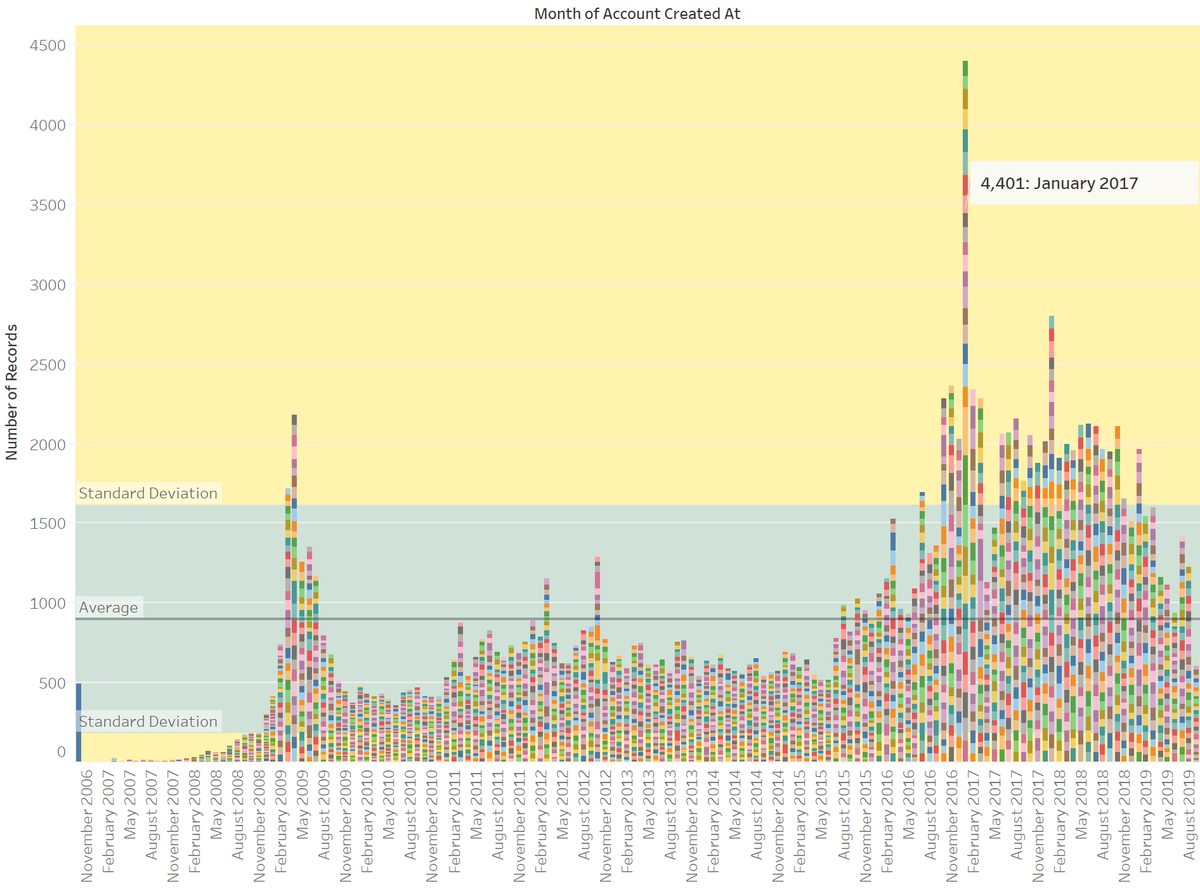
Screenshot below of guiding factors to consider.
Decision to discharge to home is a clinical one.
cdc.gov/coronavirus/20…
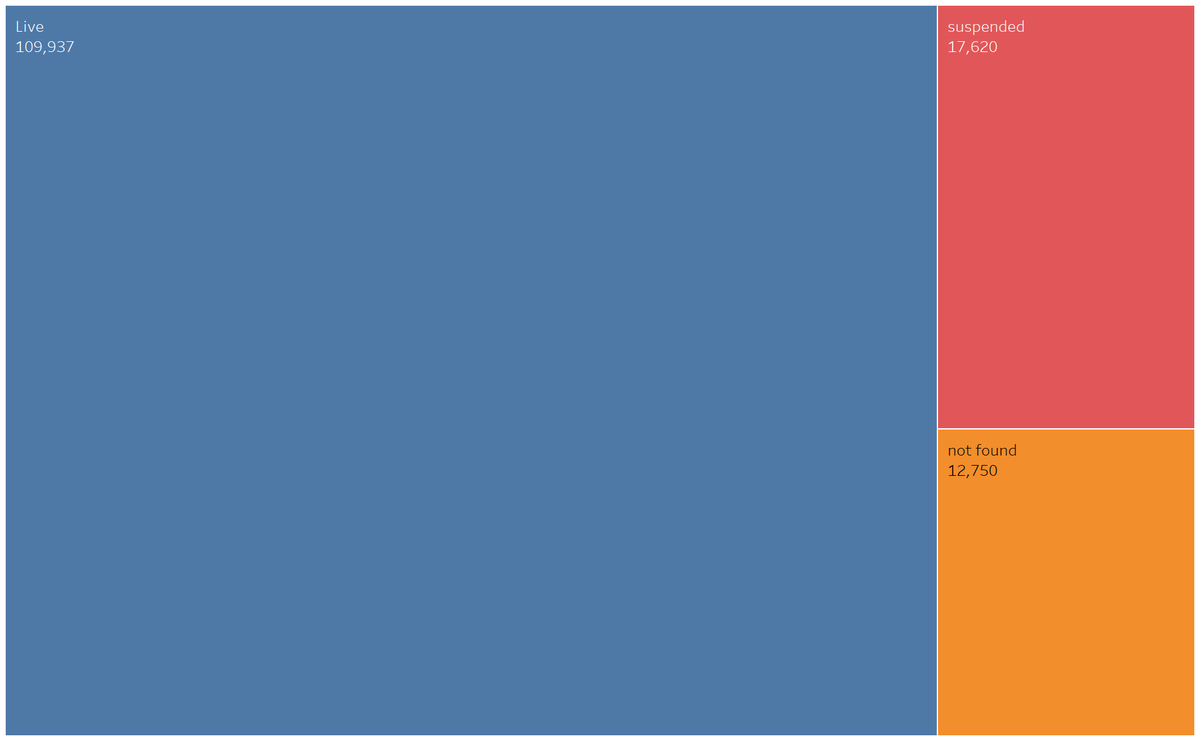
As hospital beds reach short supply, we will need to improve our turn around times on how long patients w/ #COVID19 need to actually be inpatient.
Some will get better and still require an isolation period at home after to minimize transmission.
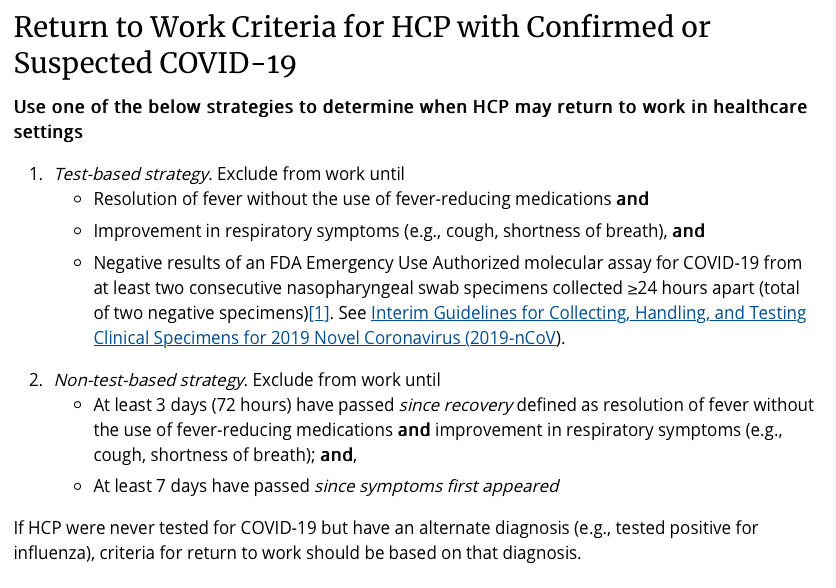
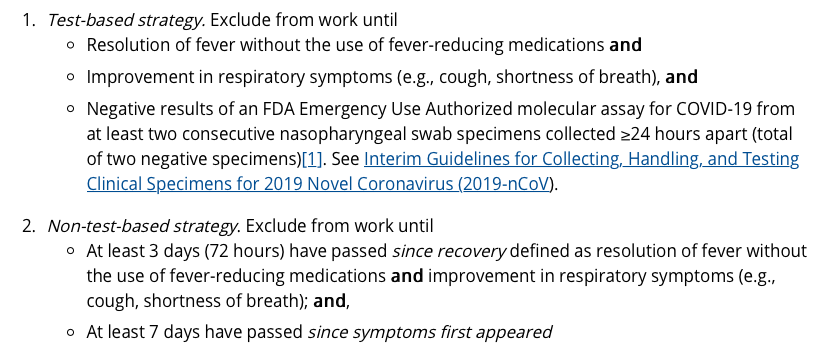
This is test-based OR non-test based. See screenshot below.
Non-test based is important while testing capacity lags.
cdc.gov/coronavirus/20…
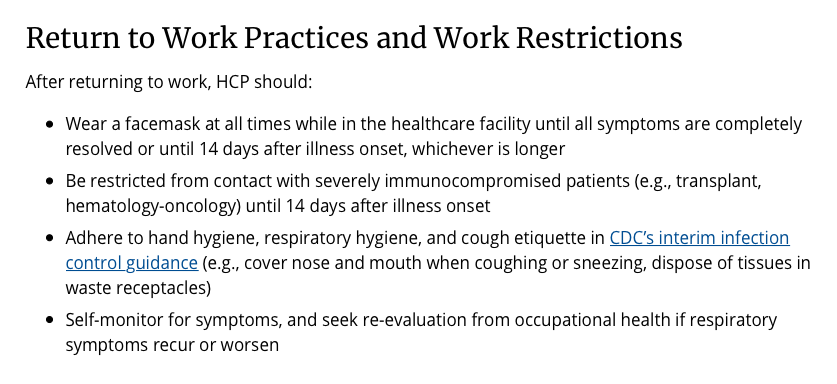
We can't afford to lose our healthcare workforce for 14 days at a time.
If we have far less transmission (even if not 0) after symptoms resolve, benefit of going back to work w/ a mask might outweigh cost.
This is the category most people will fall into.
Here, same criteria as for HC workforce except you don't need to wear a mask for 14 days once you are cleared.
Note- symptomatic v asymptomatic
cdc.gov/coronavirus/20…
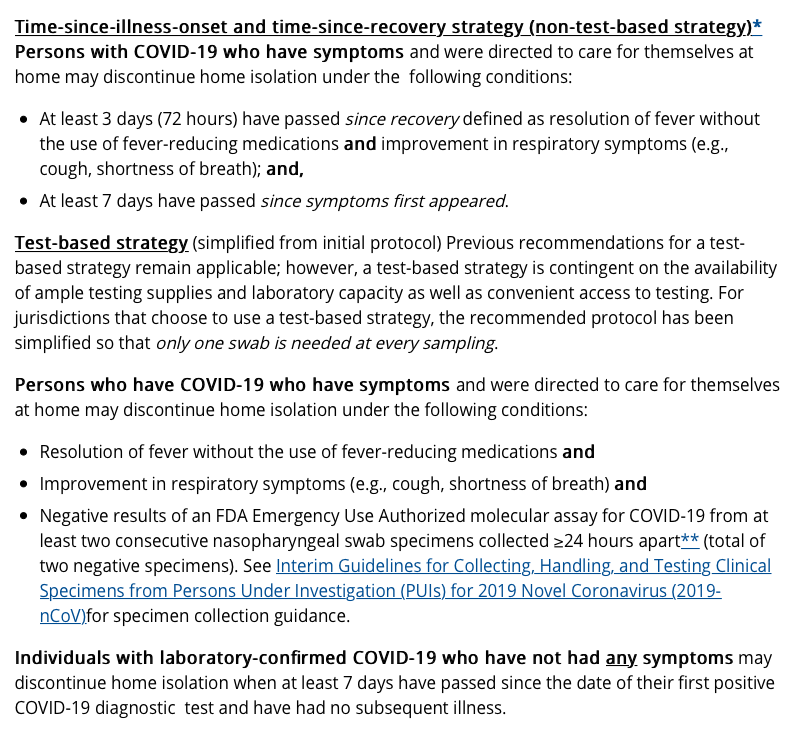
Having criteria that are not completely reliant on 2 neg PCRs is important. Consecutive PCR testing is tough on all health systems
W/ that all being said...
At some point (which honestly is probably now), we will be forced to move quickly & think w/ the mindset of:
Optimize good, minimize harm.
Uncertainty is tough. We deal w/ it as doctors all the time.
But, being paralyzed by the lack of data is also an issue.
If we do nothing at all, we are in trouble.
Everything we do will be a tradeoff.
Hardly anything comes w/o a risk.
But which risk are you willing to take?
Are you willing to risk that we missed the window to drastically curb #COVID19 because we lacked all the data?
"If you need to be right before you move, you will never win."
Remember those words.