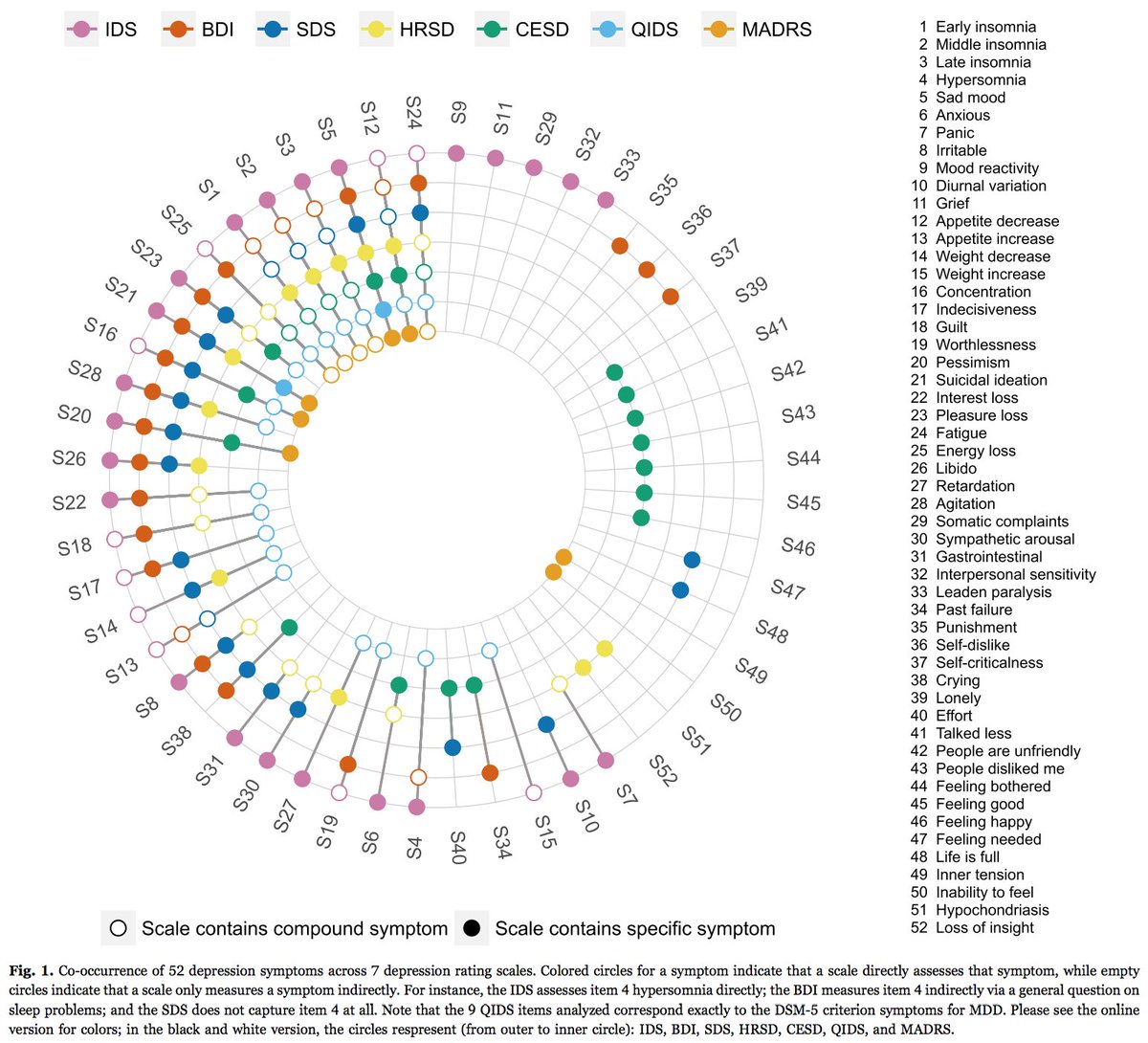
Sx = symptoms, MDD = major depressive disorder.



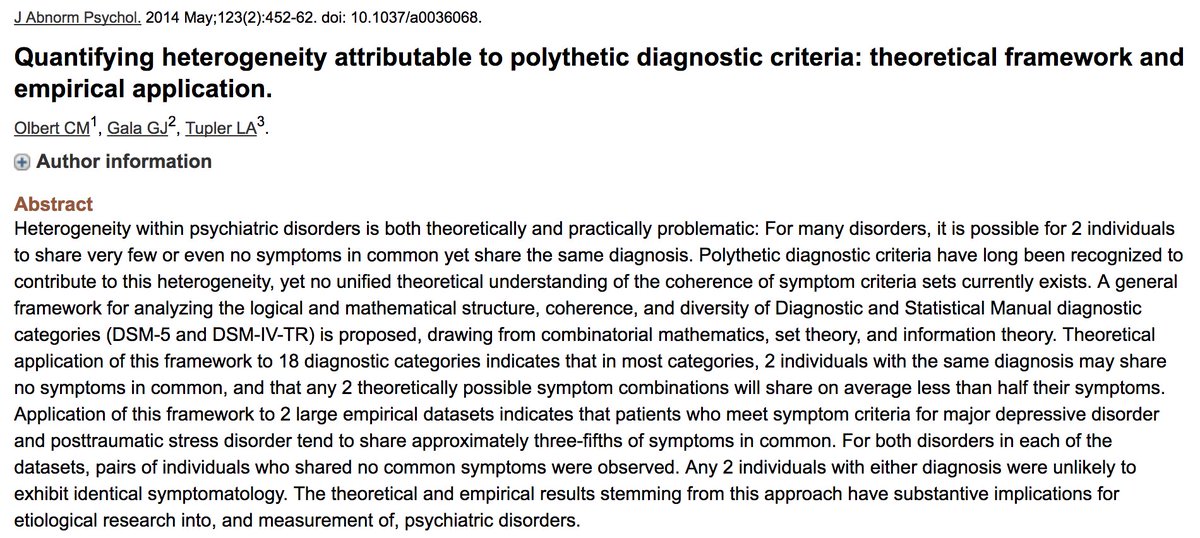
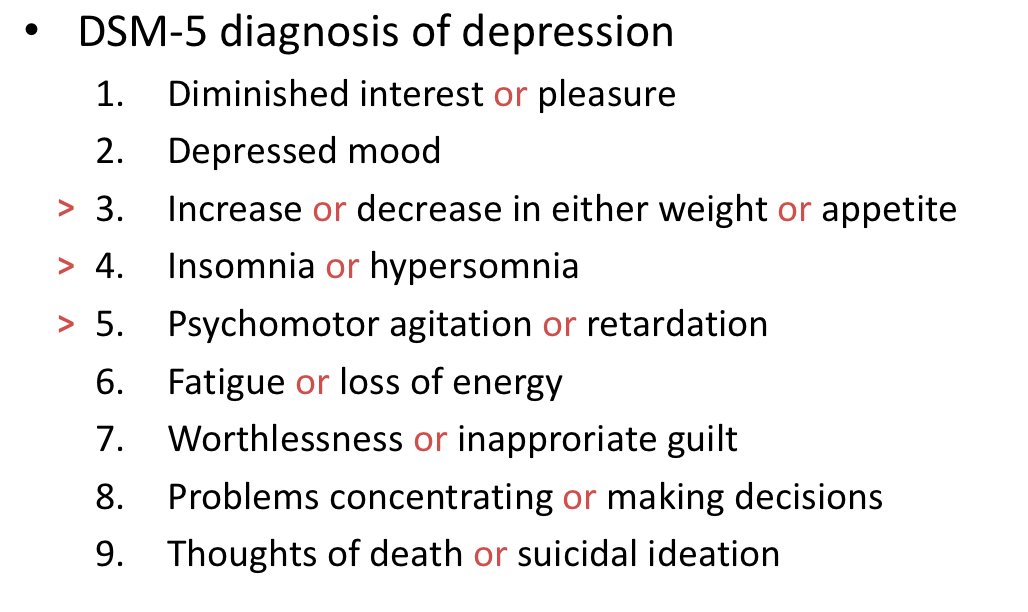
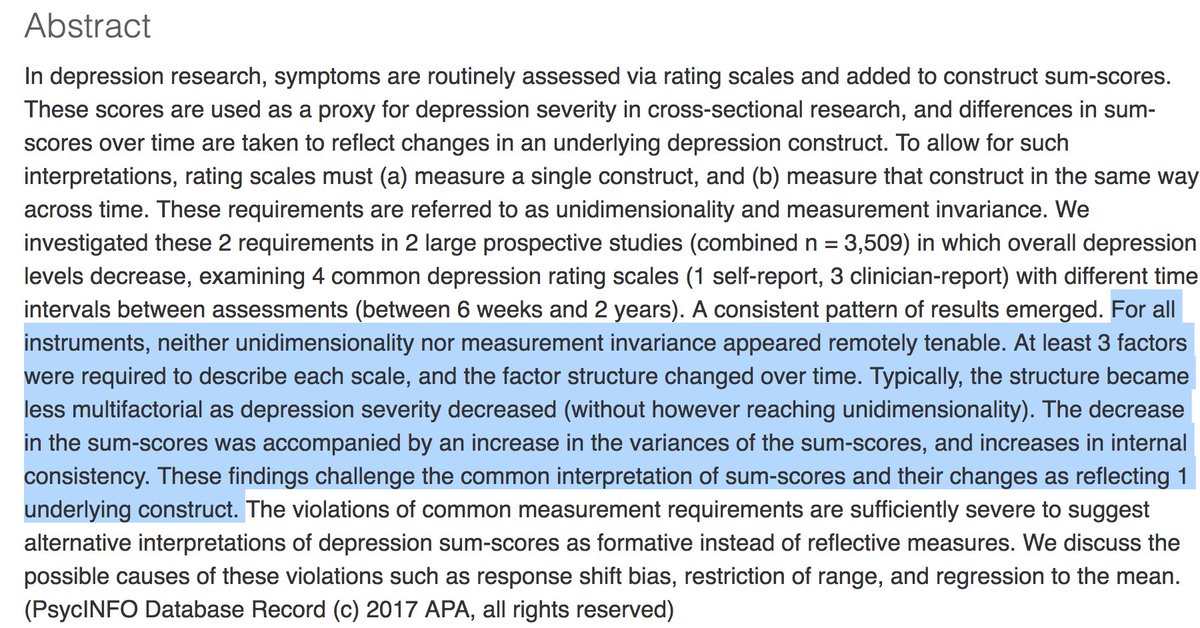
(ncbi.nlm.nih.gov/pubmed/25451401; ncbi.nlm.nih.gov/pubmed/24886017).
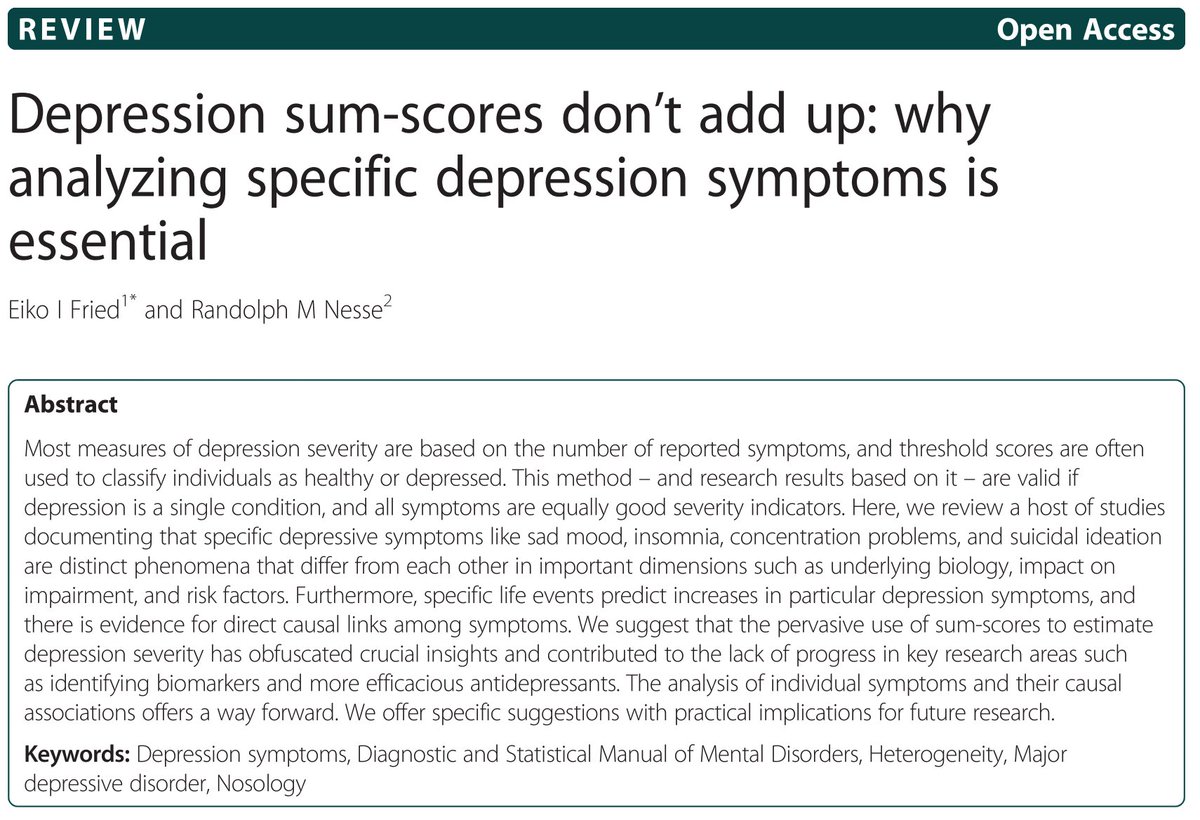
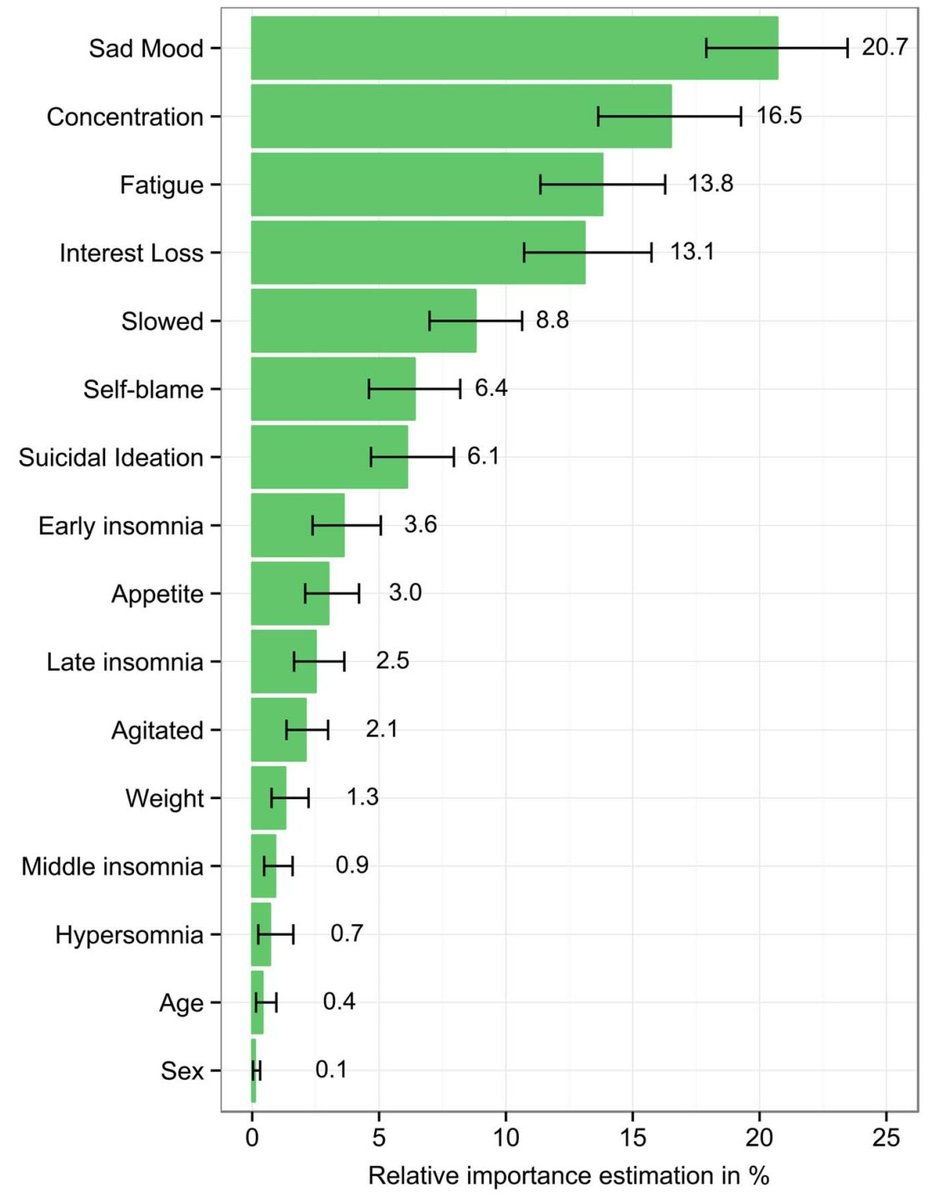
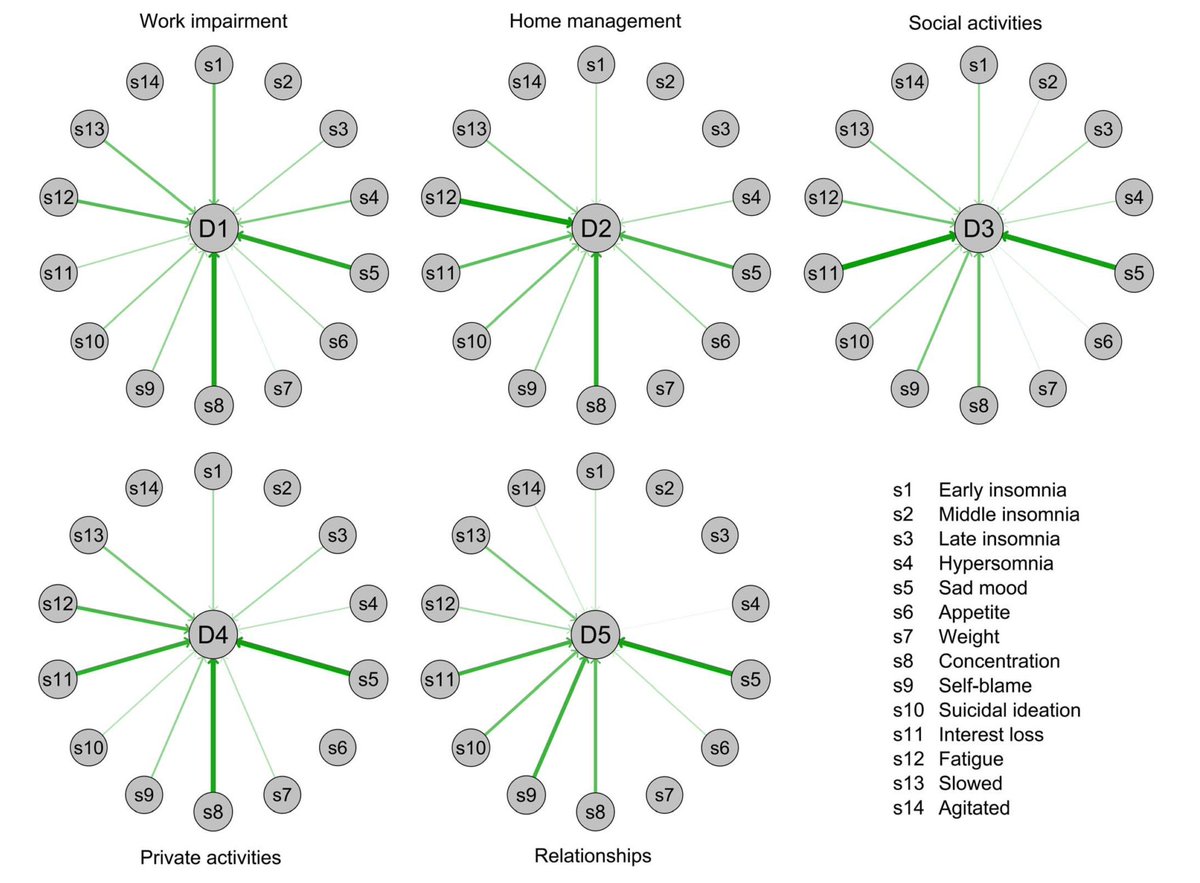
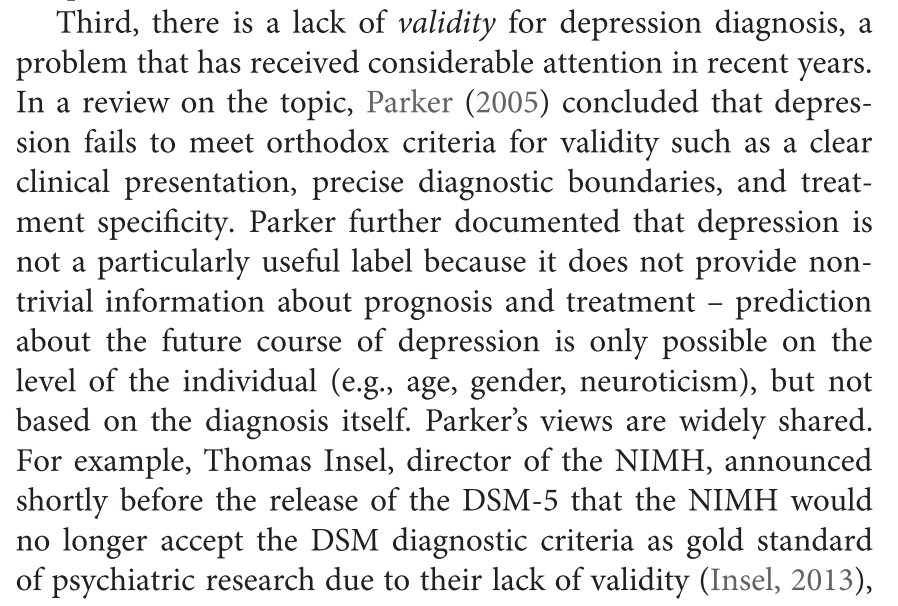
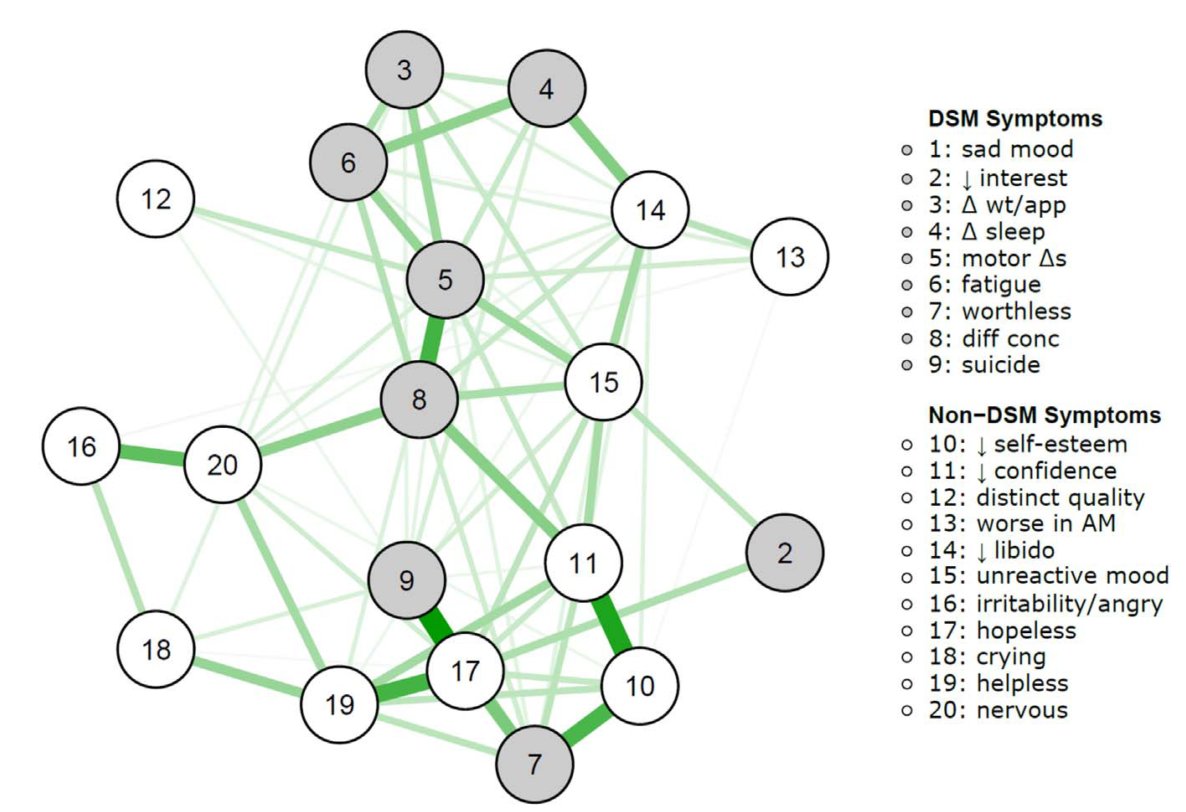
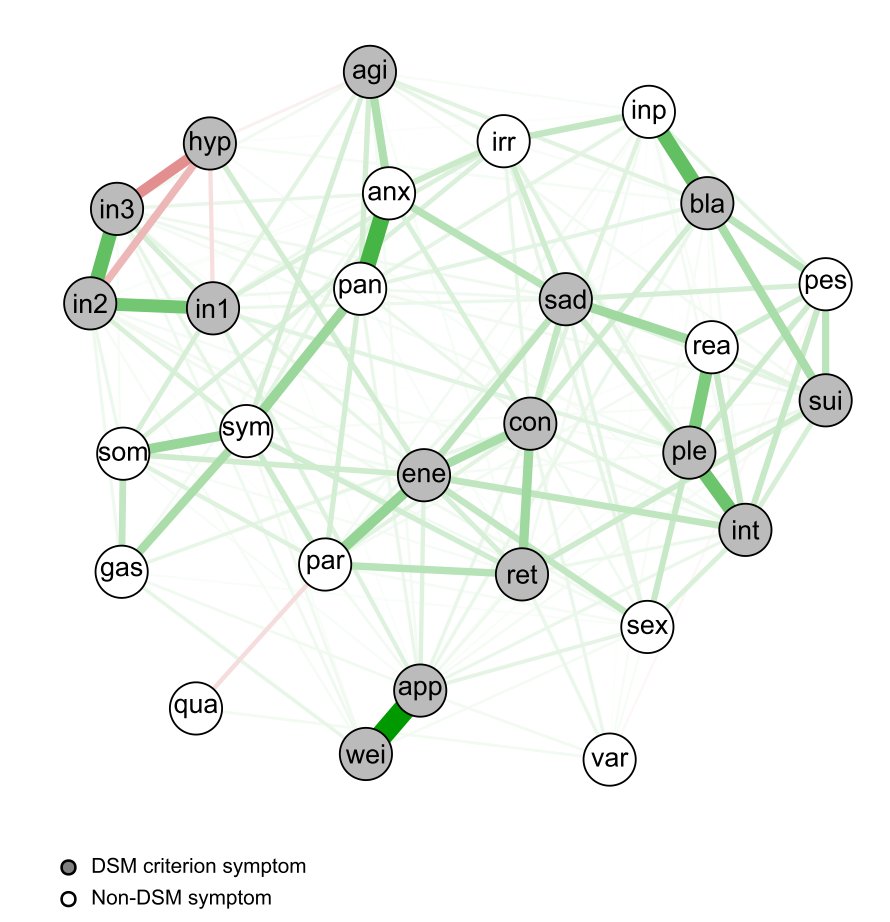
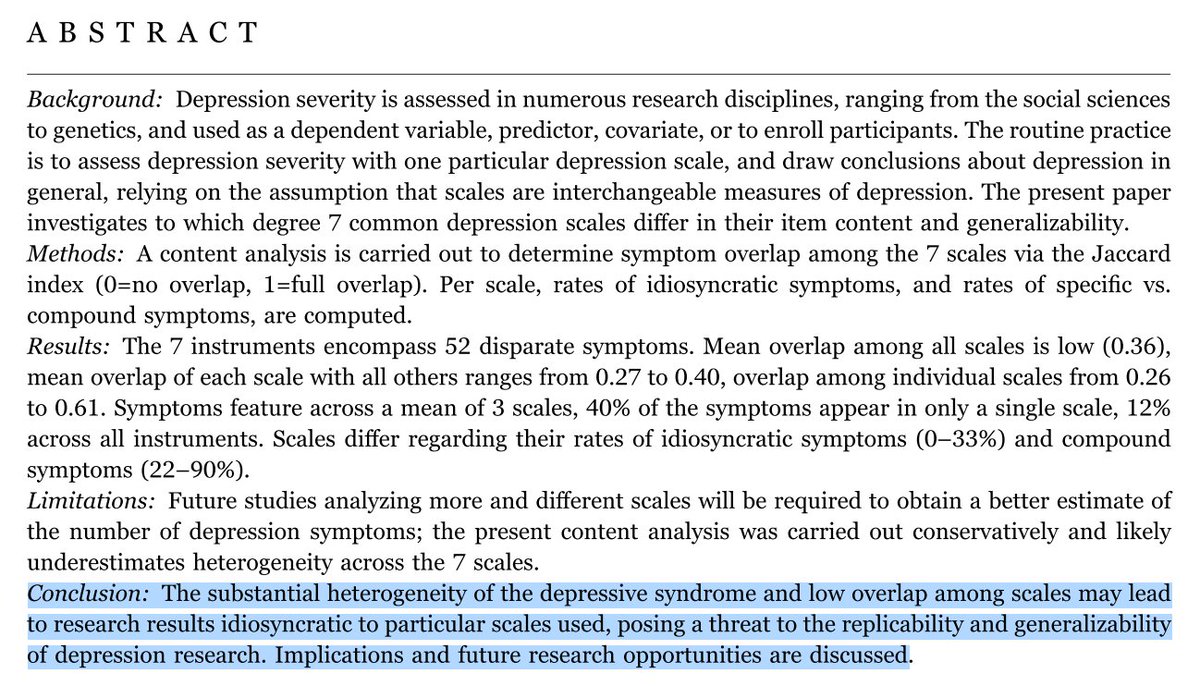
a) aggregate data from different sources that used different scales w different Sx
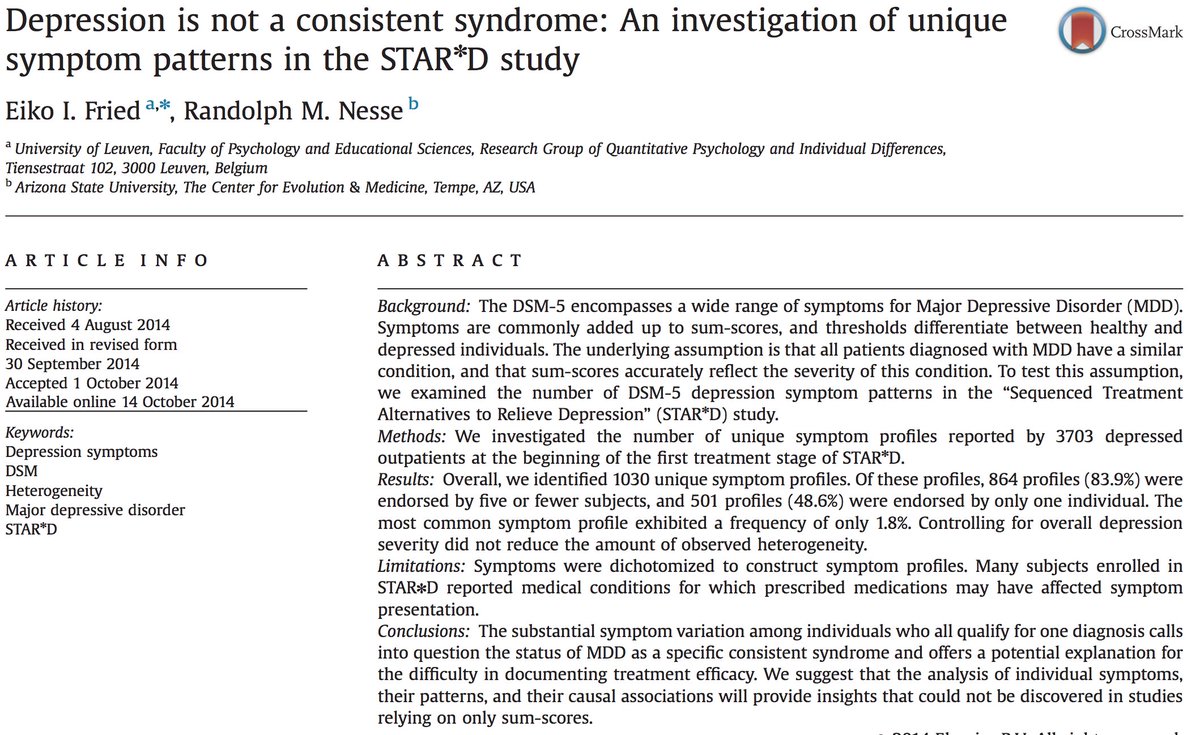
b) add Sx to sum
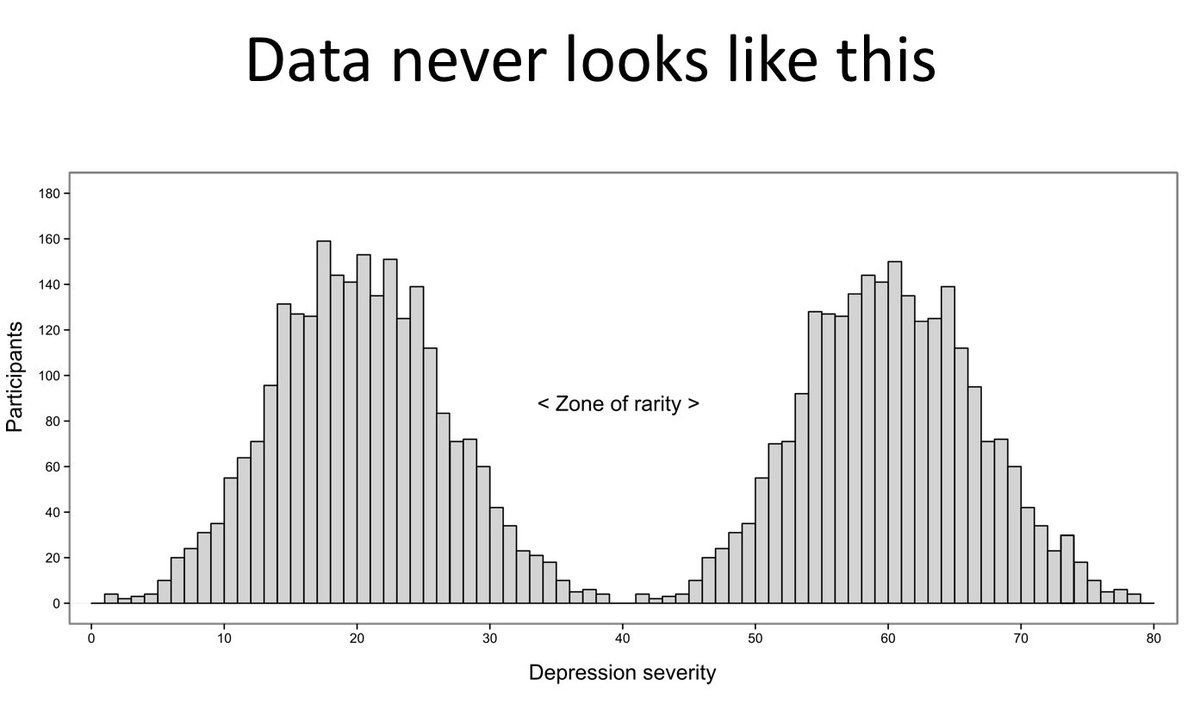
c) split on arbitrary criteria / dataset
d) correlate binary diagnosis to SNPs
Destroys nearly all information in the process.
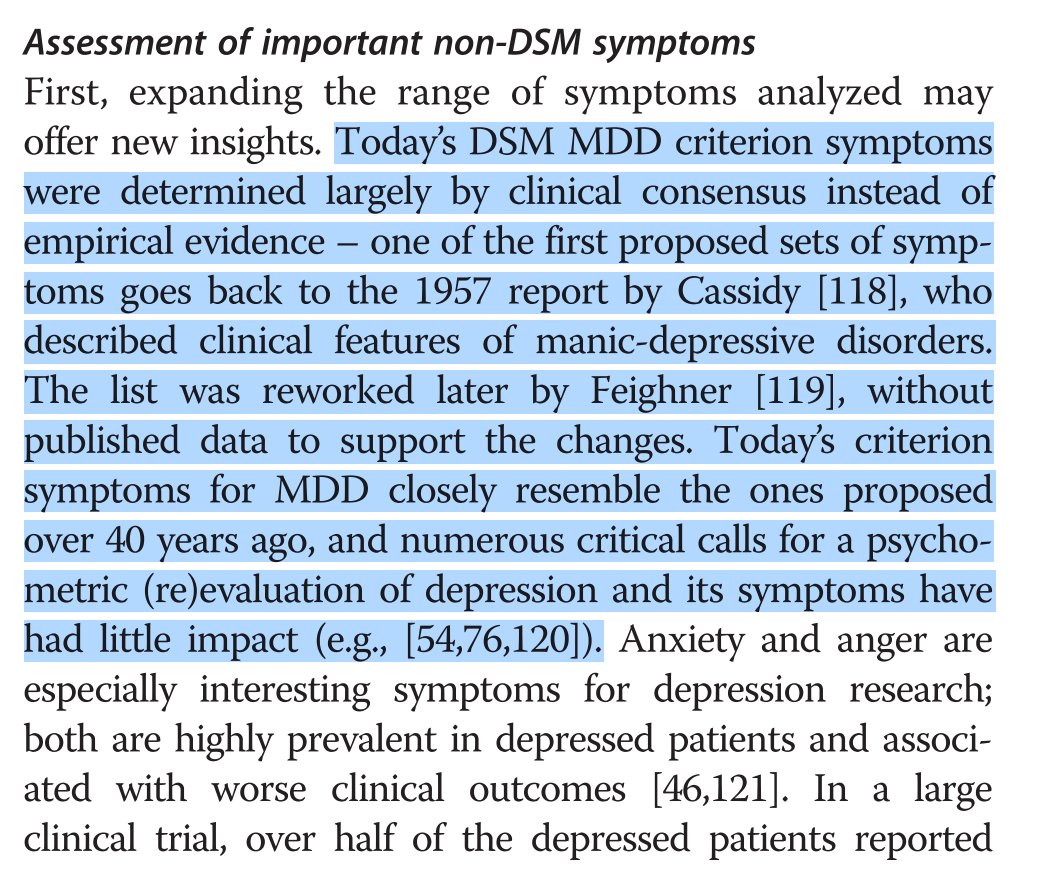
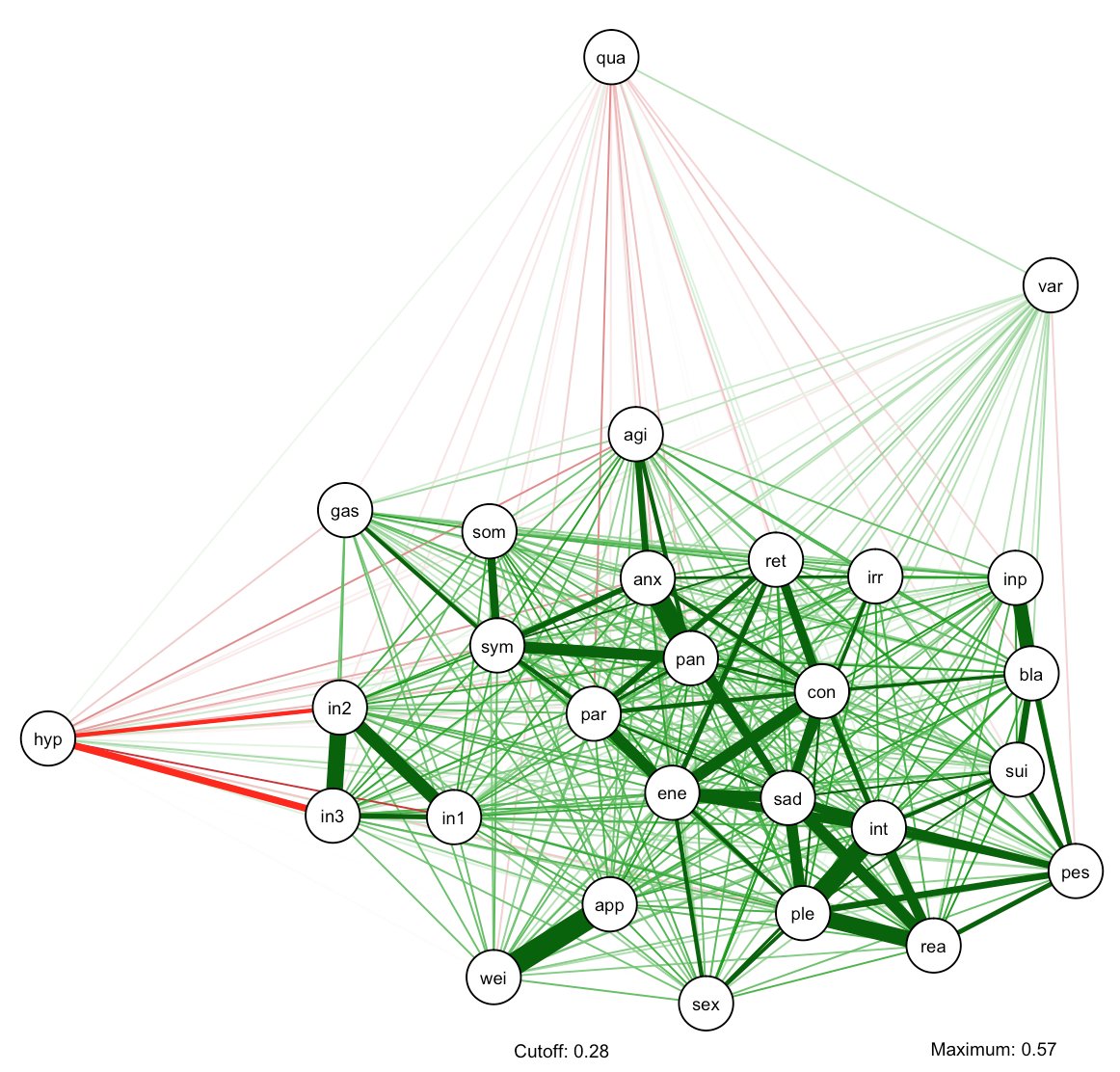
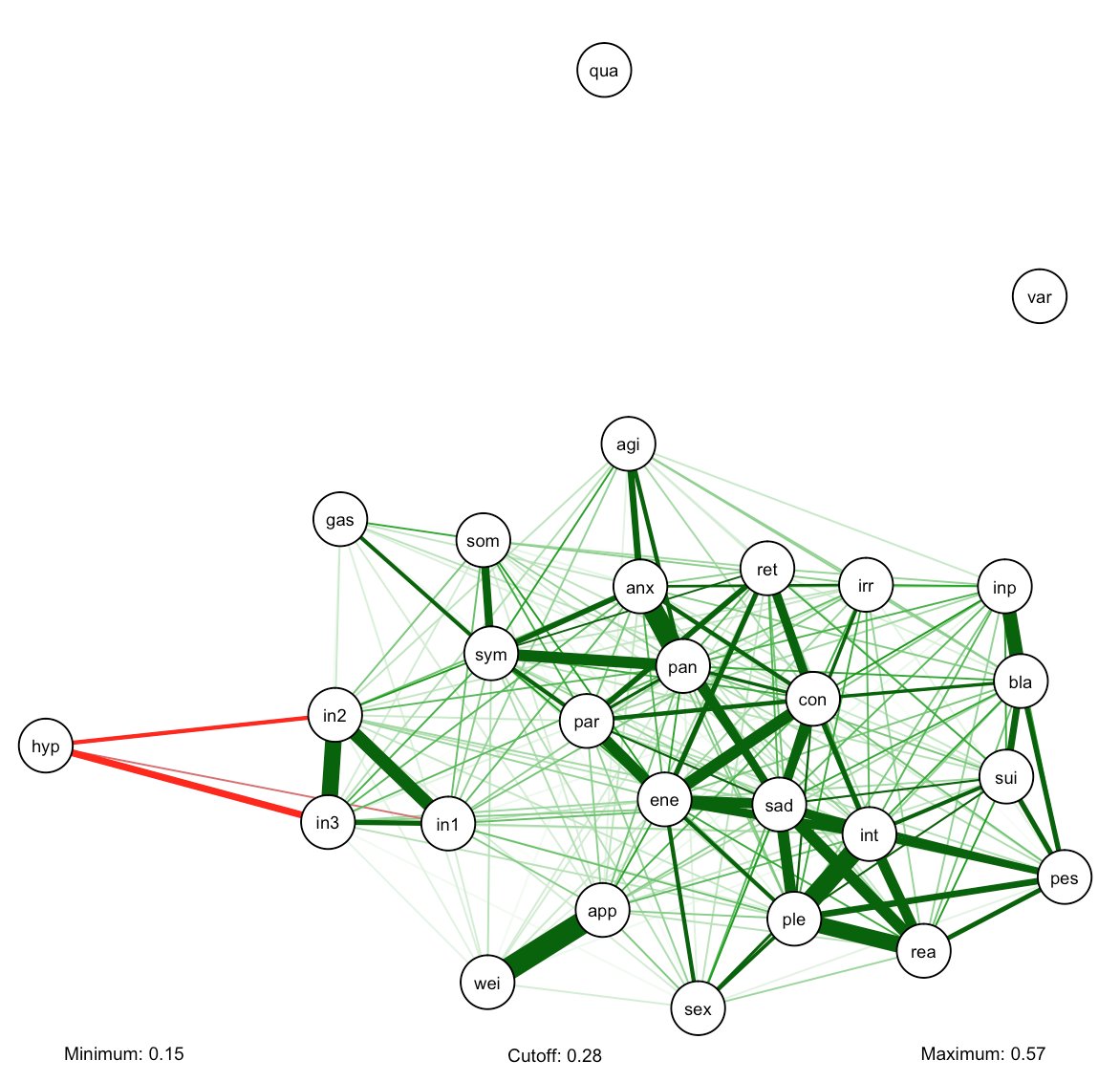
Analyze individual symptoms & use data-driven approaches to inform development of DSM-6 (frontiersin.org/articles/10.33…; tandfonline.com/doi/full/10.10…).
The end.