TL;DR:
- In SF, some ONEM visit prices run 350 - 400% of Medicare
- Employers should be cautious. Proactive primary care can cut costs, but this is not the way.
1/n
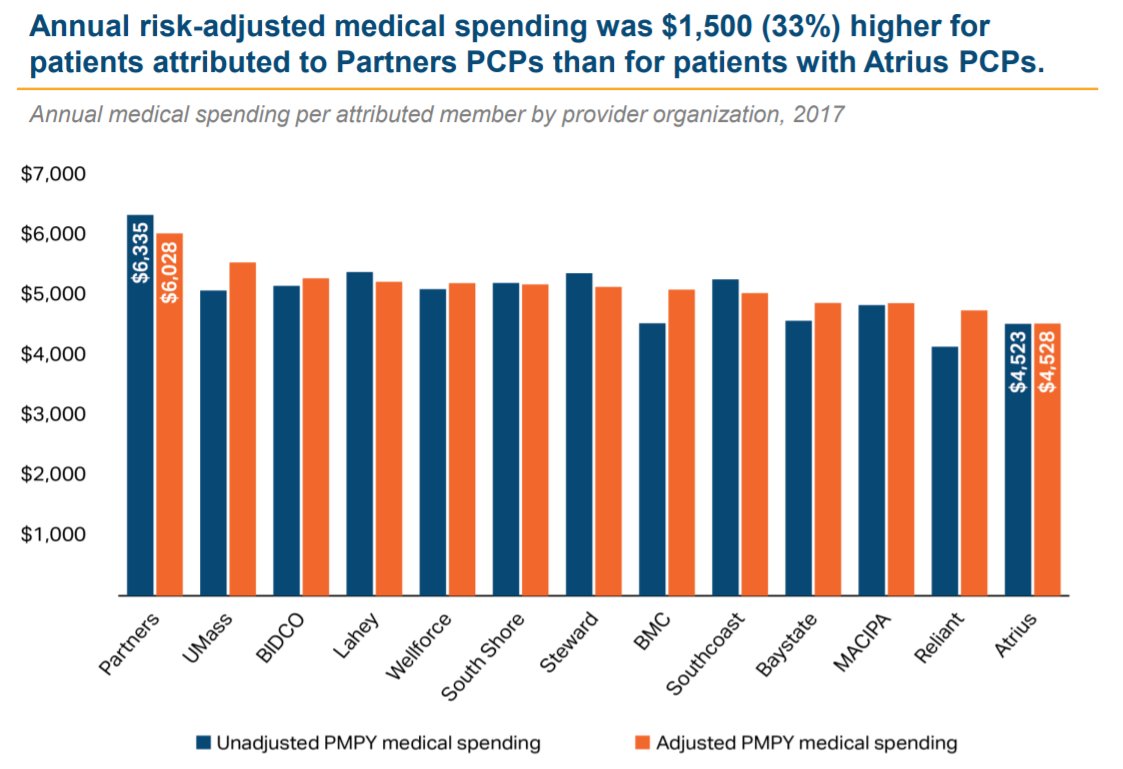
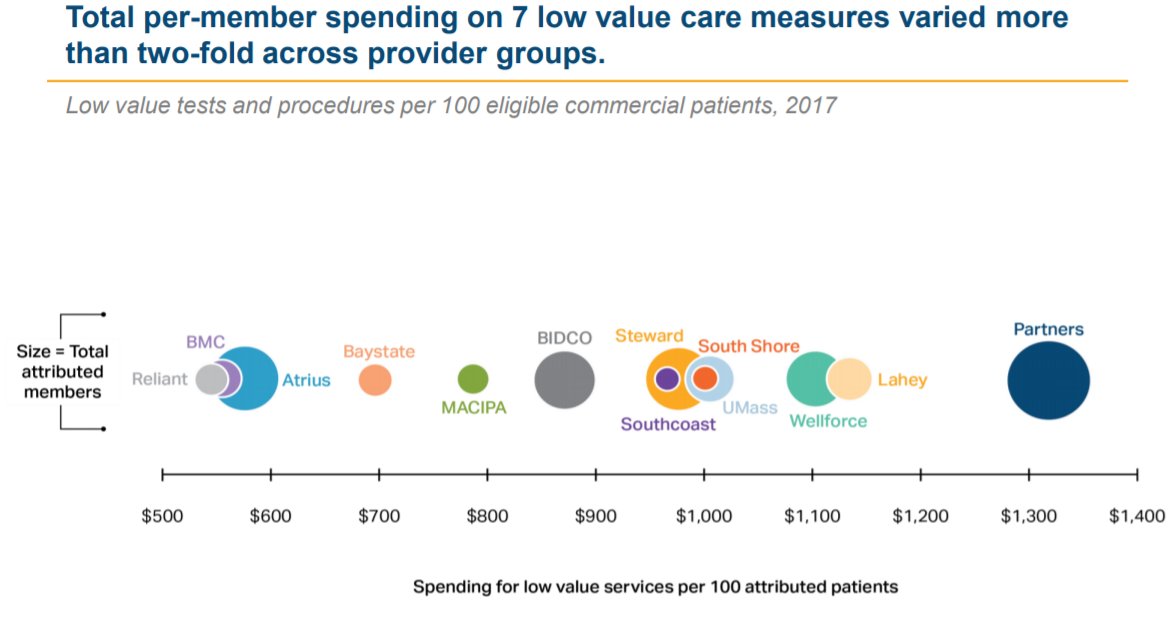
1) Evidence suggests that high-performing PCPs can save $$, even in the commercial population.
E.g. @Mass_HPC, finds risk-adjusted cost deltas up to $1,500 PMPY across medical groups, via referral patterns (i.e. secondary care prices) and low-value care
More on that here:
In short, all-in cost for this one <15-min visit was $460, plus $138 for routine lab tests.
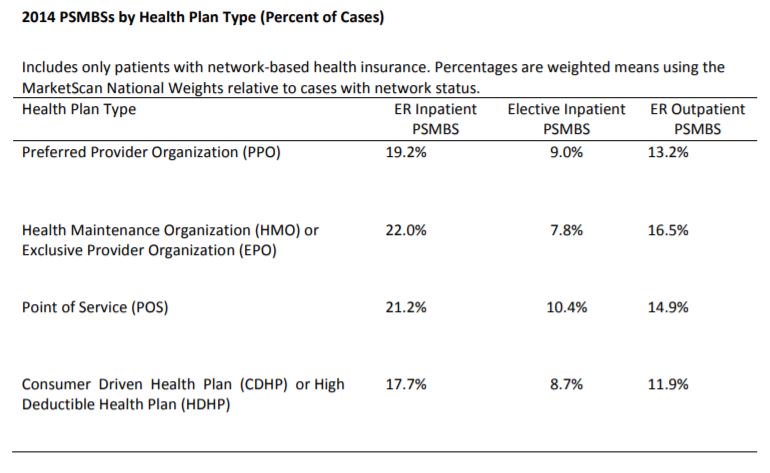
Receipts (h/t to @HealthCostInst):
[checks notes]
1,500% of Wal-Mart.
Debatable to reimburse this at all. Per Anthem, for example, 36415 is not eligible for separate reimbursement on top of a routine E/M ofc visit.
In any case, Medicare pays $3, (its 5 mins of phlebotomist time). So... ~400% of Medicare.
Feels like upcoding - given the lack of a problem, Dx or preventive counseling, it arguably should be coded as 99212/3.
And the price is just inexplicably high. Bay Area AMCs (UCSF, Stanford etc) charge 200-300% of Medicare for inpatient care.
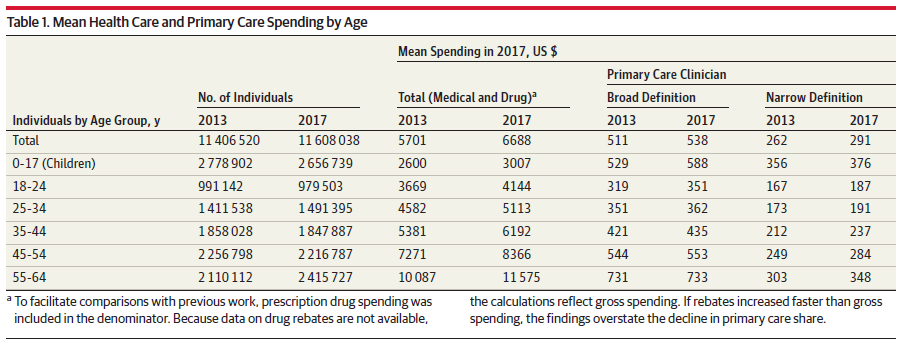
At prices this high, sending staff to ONEM could double or triple their primary care spend (assuming ~2.5 visits PMPY). And then, referral relationships w/ high-cost secondary care will eliminate one of the best savings vectors.
But if the baseline ED utilization is 0.2 - 0.3 ED visits PMPY at, say, $1,400 a pop, there are just not enough avoidable ED visits to offset the additional outlays on high-priced primary care.
All-in, while I'm a fan of investing in primary care, it is hard to see how this revenue model works for employers. /n