@sanjayvdesai @OslerResidency @JHUPCCMFellows @CPSolvers @thecurbsiders @cardionerds @tony_breu @david_furfaro @chadhoc
ncbi.nlm.nih.gov/pubmed/?term=1…
ncbi.nlm.nih.gov/pubmed/3383620
ncbi.nlm.nih.gov/pubmed/2347780
ncbi.nlm.nih.gov/pubmed/19487931
ncbi.nlm.nih.gov/pubmed/?term=8…
ncbi.nlm.nih.gov/pubmed/?term=2…
ncbi.nlm.nih.gov/pubmed/?term=3…
ncbi.nlm.nih.gov/pubmed/?term=3…
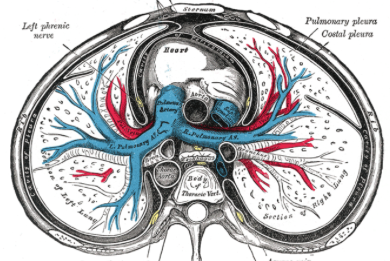
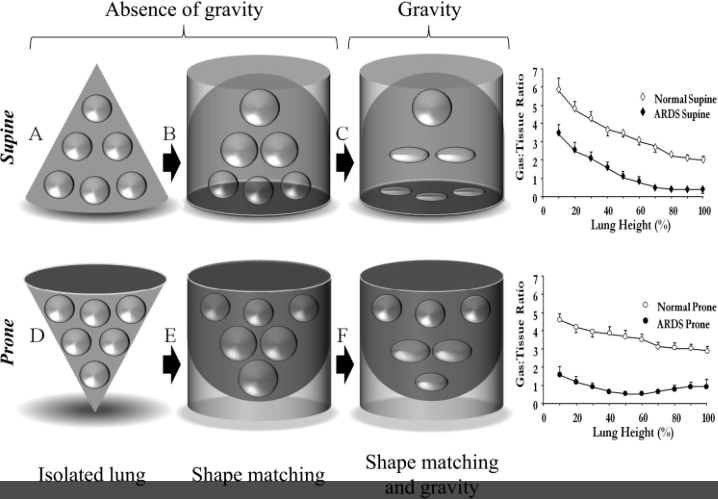
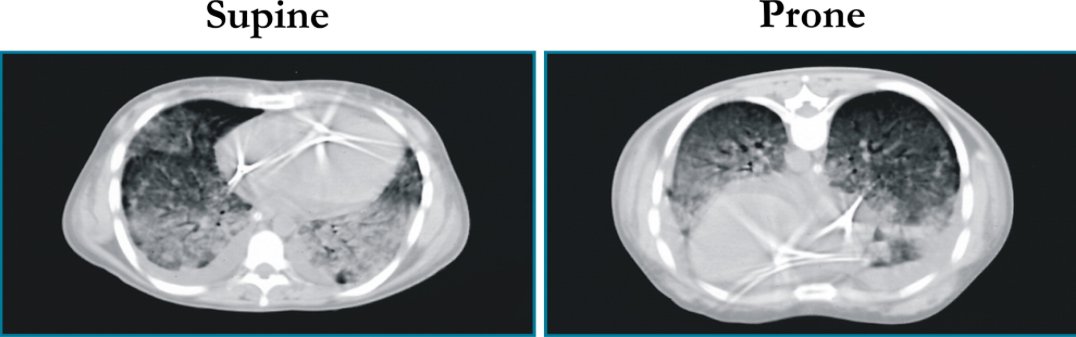
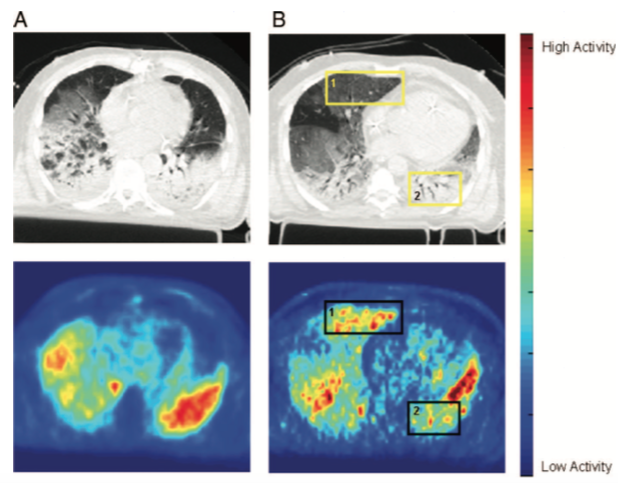
✅ Prone positioning (PP) leads to more homogenous inflation of lungs
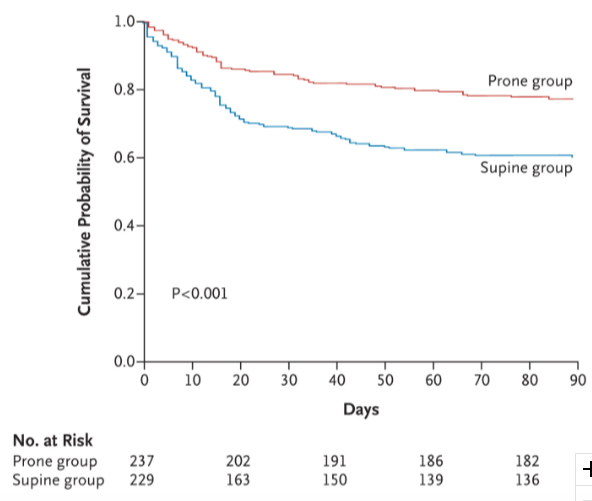
✅ This improves oxygenation, and reduces mortality in severe ARDS
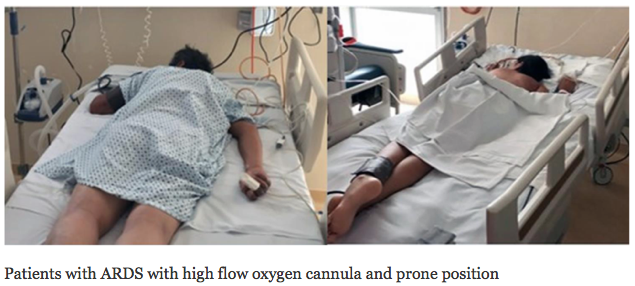
✅ HFNC & PP is a possible strategy to consider to avoid intubation (especially in COVID pandemic), but more studies are needed