Here's what I found. #thread
1/
What evidence do we have on this, and further, what evidence do we have on strategies that mitigate these mental health issues in health care workers?
I presented these data the @UChicagoMed @UCCancerCenter grand rounds last week.
2/
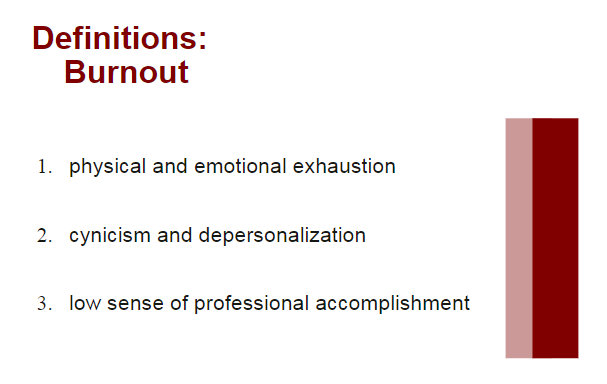
Burnout, initially described by Dr. Maslach as the prolonged physical and psychological exhaustion related to a person's work. Not specific to medicine, although the definition has been honed for medicine (see slide). #burnout
3/x
Enter: compassion fatigue (= burnout + secondary traumatic stress). Better definition for what health care workers experience.
5/
Short story: it's complicated.
Long story: keep following the #thread. #burnout #ptsd
7/
Initial definition: “a betrayal of what’s right, by someone who holds legitimate authority, in a high-stakes situation.” #moralinjury
8/
statnews.com/2018/07/26/phy…
In short: #burnout doesn't reflect systemic pressures that affect mental health of health care workers.
9/
"the challenge of simultaneously knowing what care patients need but being unable to provide it due to constraints that are beyond our control"
ncbi.nlm.nih.gov/pmc/articles/P…
10/
Theoretically, this makes sense. However...
11/
Further, which comes first? Moral injury --> compassion fatigue? Burnout --> moral injury? How are they related?
12/
Now, we transition this #thread to historical precedents, specifically SARS.
13/
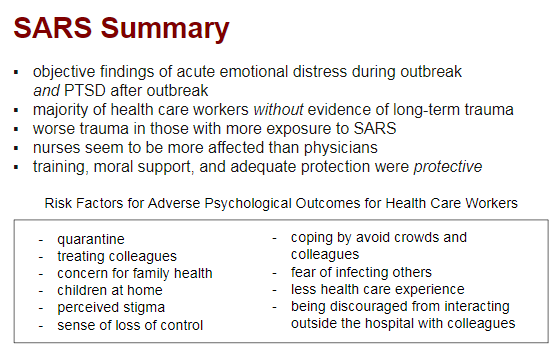
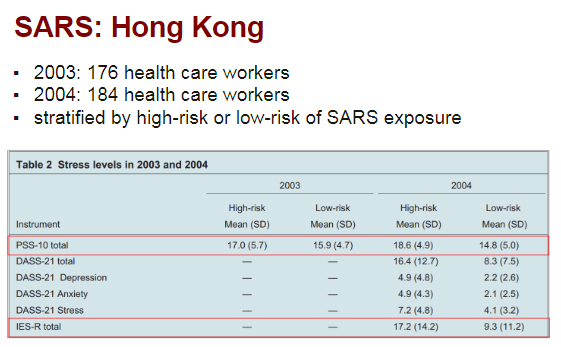
Although only ~8000 cases worldwide of #SARS back in 2003, many similarities in transmission, high nosocomial spread, and use of #quarantine in China and Canada.
14/
#covid4mds #moralinjury #SARSCoV2 #foamcovid
15/
- High-risk and low-risk workers both had high acute and chronic stress.
- Chronic stress increased 1 year later in high-risk workers.
- #PTSD higher in high-risk.
ncbi.nlm.nih.gov/pubmed/17500305
16/
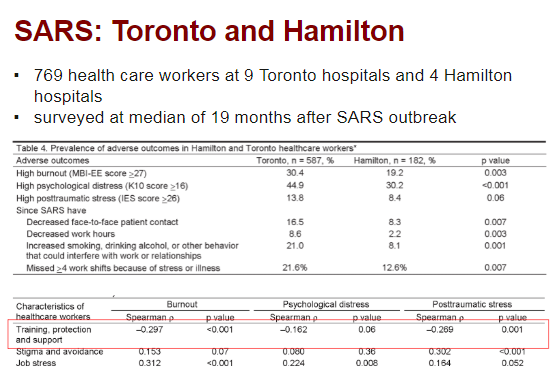
- High #burnout & #PTSD >1 year after outbreak, worse if exposed to SARS pts.
- Adequate PPE and support = less burnout & PTSD.
ncbi.nlm.nih.gov/pubmed/17326946
17/
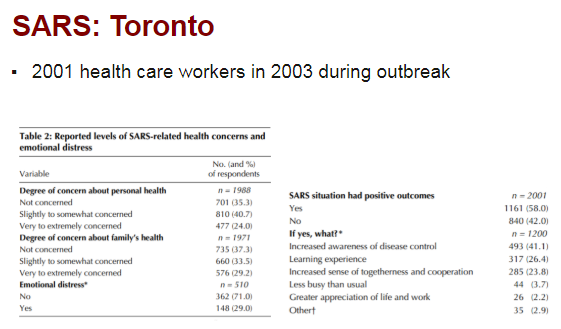
- 30% acute emotional distress in health care workers.
- 45% nurses, 33% allied HC professionals, 17% physicians with acute distress.
- 58% felt SARS has positive outcomes (see slide).
ncbi.nlm.nih.gov/pubmed/14993174
18/
Adequate training, PPE, and feeling of support were PROTECTIVE of poor mental health outcomes for health care workers.
The first inkling from the literature that structural / organizational efforts have efficacy.
20/
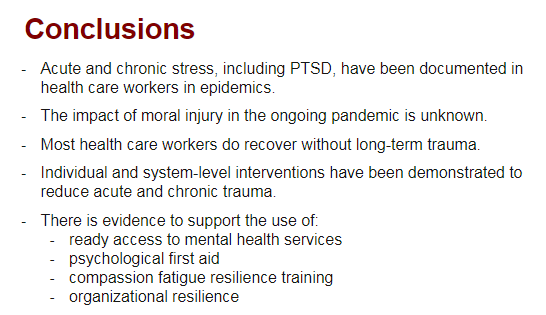
First, a good thing: the majority of health care workers *just get better* with respect to both acute and chronic stress.
However, chronic stress leads to attrition out of patient care (see Toronto/Hamilton study in #thread).
21/

Much more widespread, more limitations on resources for health care worker protection AND patient care (#PPE, #ventilatorshortage) --> potentially more moral injury?
This needs research in current #pandemic.
22/
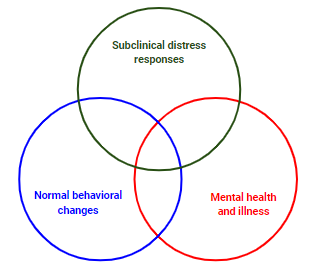
#mentalillness during and after pandemics.
My next goal was to find evidence-based strategies for mitigation of these moral and emotional insults.
The #thread continues with that research.
23/
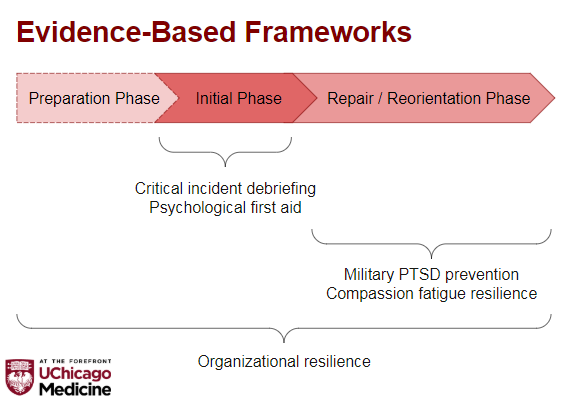
I overlaid the evidence-based frameworks on top.
Remember: different ares will be at different points on this timeline.
cambridge.org/core/services/…
24/
Long story short: super controversial, and meta-analyses have showed that it may actually INCREASE risk of #PTSD.
jenonline.org/article/S0099-…
25/
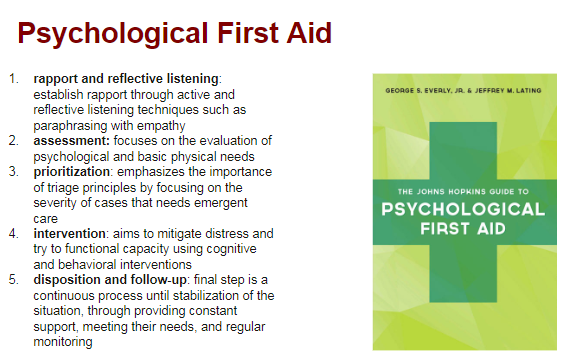
Anyone can learn to do it, too! Not just mental health workers: apa.org/practice/progr…
28/
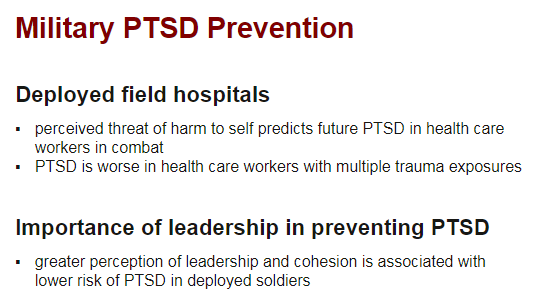
However, important to note that *perceived threat of harm* predicts development of PTSD rather than just exposure.
30/
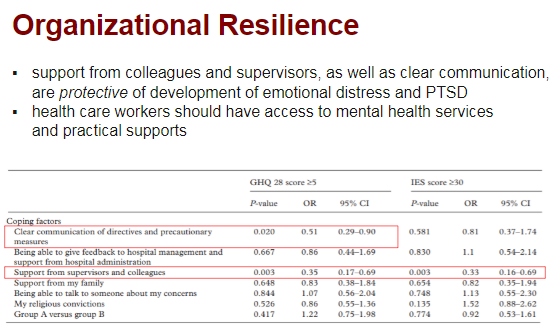
Adding to this assertion is the finding in military literature that strong, compassionate leadership is also *protective* against development of #PTSD.
32/
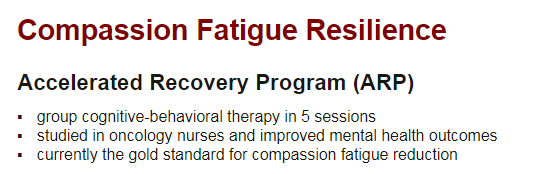
The Accelerated Recovery Program, developed in the 1990s, is a group CBT-approach to reducing CF & #PTSD, with efficacy demonstrated in nurses.
However, has not been studied in epidemic setting.
33/
I know this #thread is getting long, but I want to really spend some time on the evidence that supports organizational interventions in protecting HC worker mental health.
34/
It refers to an system-wide approach that provides for *all* of the needs of health care workers (mental AND physical) during crises.
ncbi.nlm.nih.gov/pmc/articles/P…
35/
This adds to the existing military literature that leadership is protective against PTSD.
36/
But, that's not all. #thread
37/
- adequate #PPE
- hazard/overtime pay
- housing/childcare support
- access to groceries/food
- scrubs
- timely mental health services if needed
38/
ORGANIZATION-LEVEL SUPPORT OF HEALTH CARE WORKERS IS A MENTAL HEALTH INTERVENTION.
The literature I cited supports this assertion. Yes, individual-level #burnout and #compassionfatigue tools are important, but...
39/
How #moralinjury plays into this is completely unknown.
40/
Modern health care has never seen this type of trauma before, and dedicated study of #moralinjury, as well as #burnout, #compassionfatigue and #PTSD in health care workers is warranted.
41/