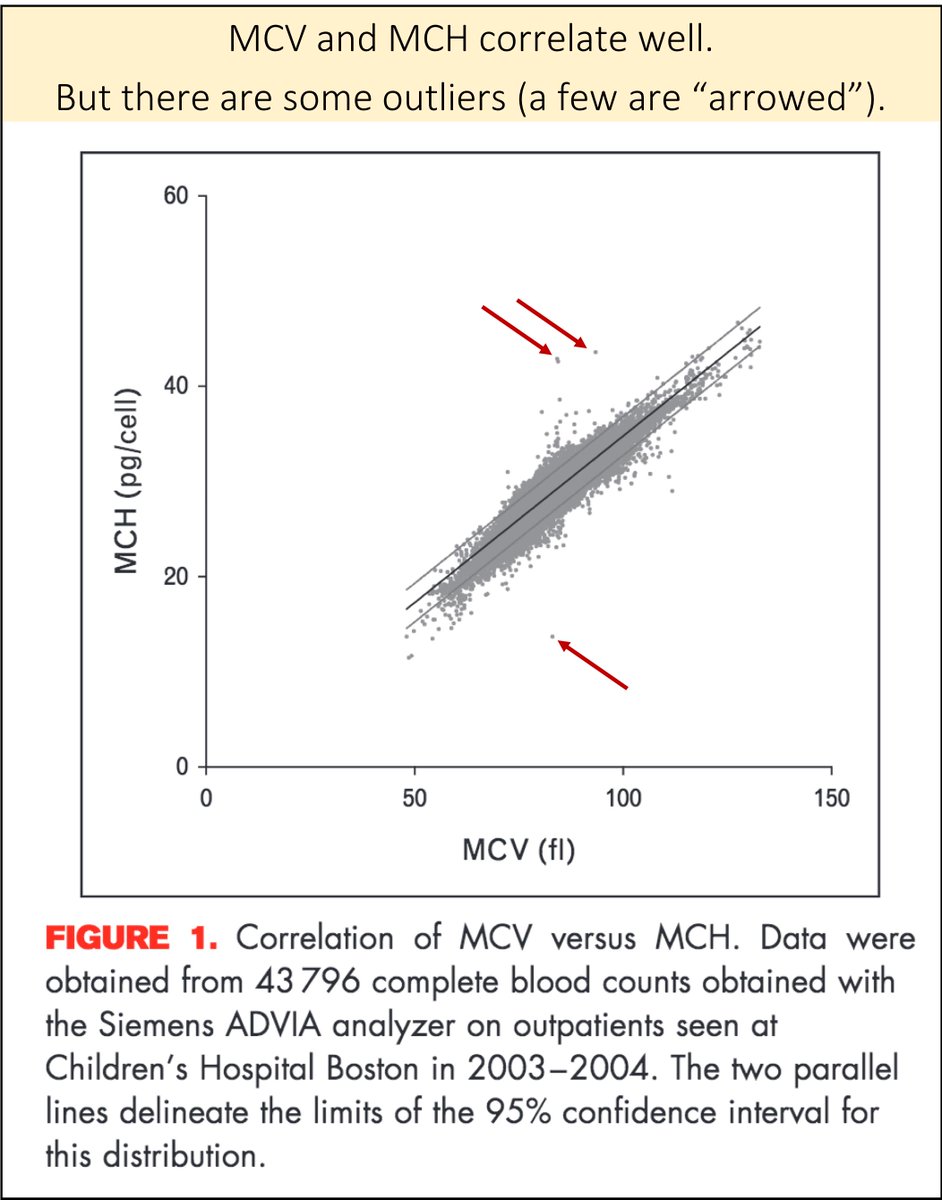
Before discussing ITP specifically, it's worth noting a 1962 paper examining rates of hemorrhage at various platelets counts in patients with leukemia.
Do you see a "threshold" level of platelets at which bleeding increases?
ncbi.nlm.nih.gov/pubmed/13897369
Though I could find no specific evidence that the risk of hemorrhage is lower in ITP than in those with bone marrow suppression, this is generally felt to be the case.
Which of the following is generally true of ITP, compared with bone marrow suppression?
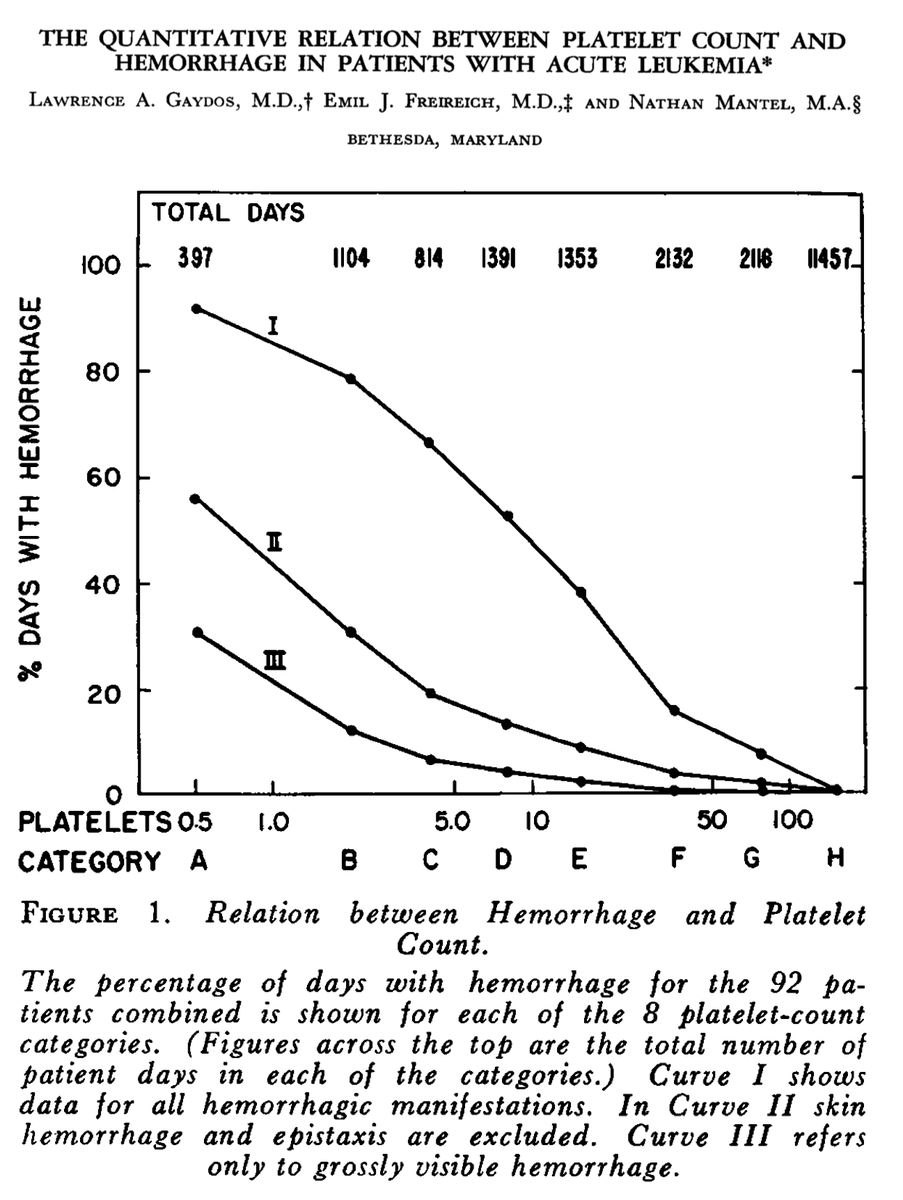
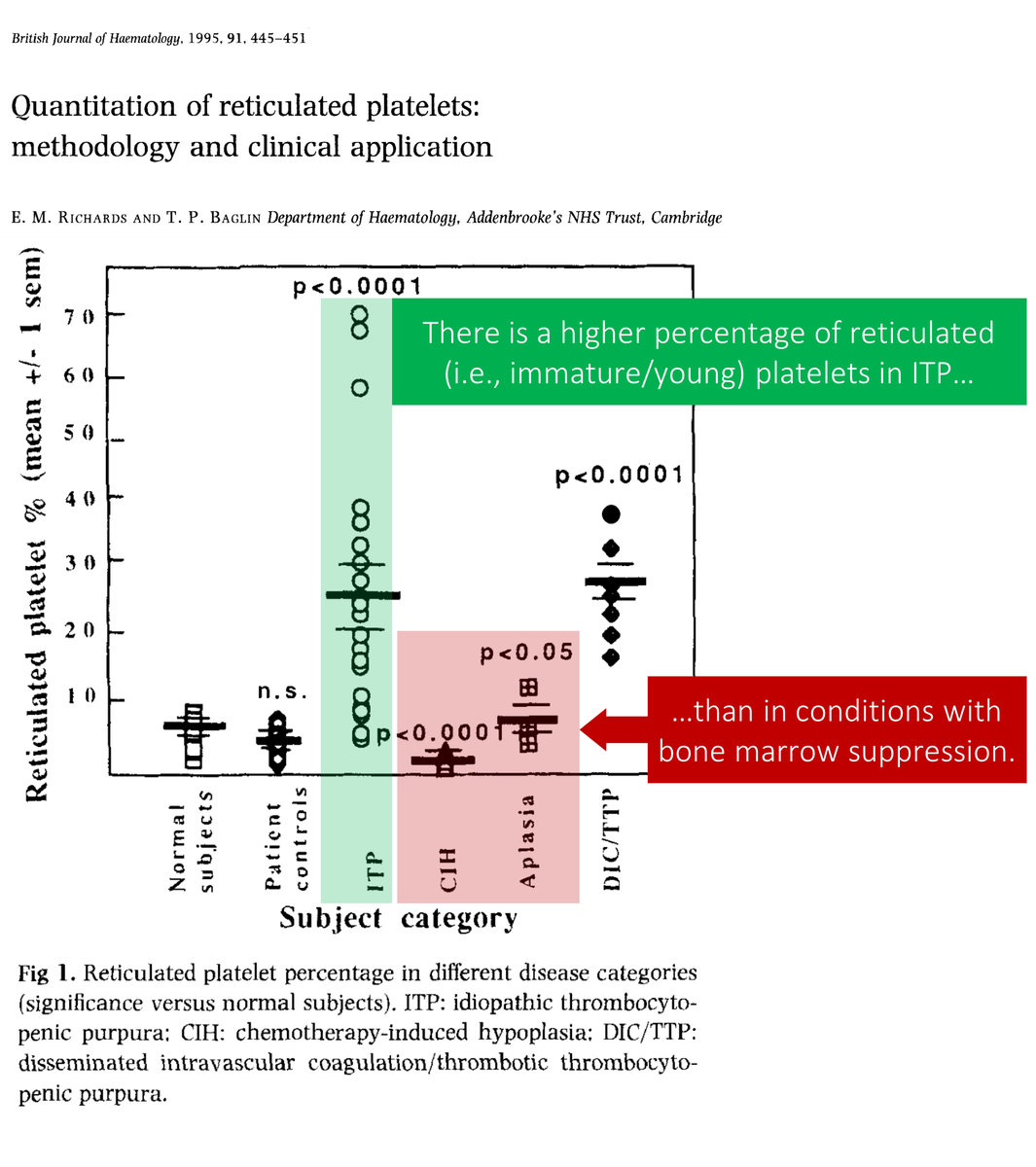
The key pathologic event in ITP is peripheral platelet destruction.
In response, the bone marrow produces new platelets. These young, reticulated (i.e., immature with stained RNA) platelets are more common in ITP than in bone marrow suppression.
ncbi.nlm.nih.gov/pubmed/8547092
Is there another condition that leads to new platelets?
Hemorrhage!
In acute hemorrhage, the bone marrow churns out new RBCs and platelets. Interestingly, in 1942, Helen Wright noted that the platelets produced in acute hemorrhage were "stickier".
onlinelibrary.wiley.com/doi/abs/10.100…
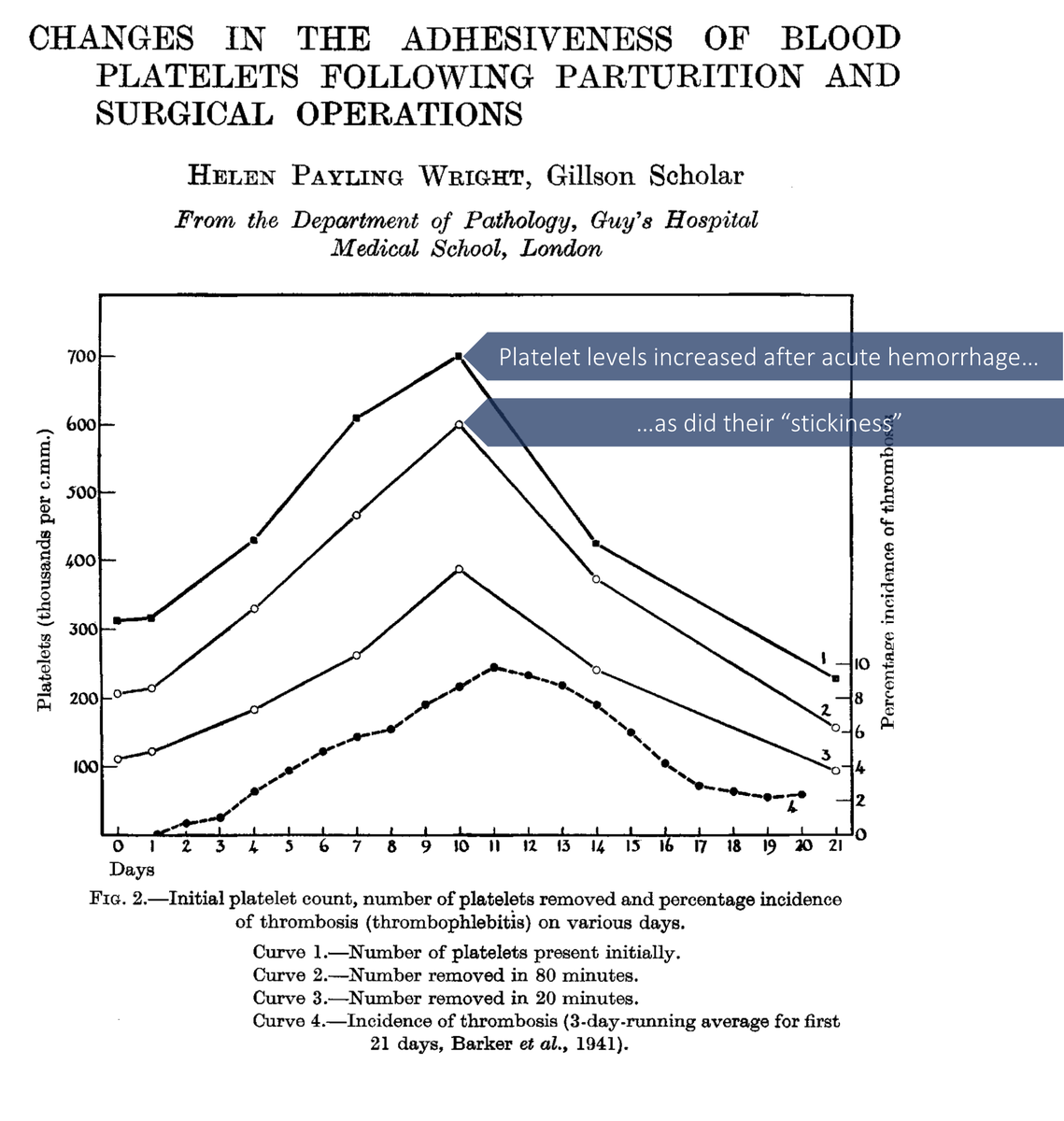
Subsequent studies confirmed the "stickiness" (i.e., superior function) of younger platelets.
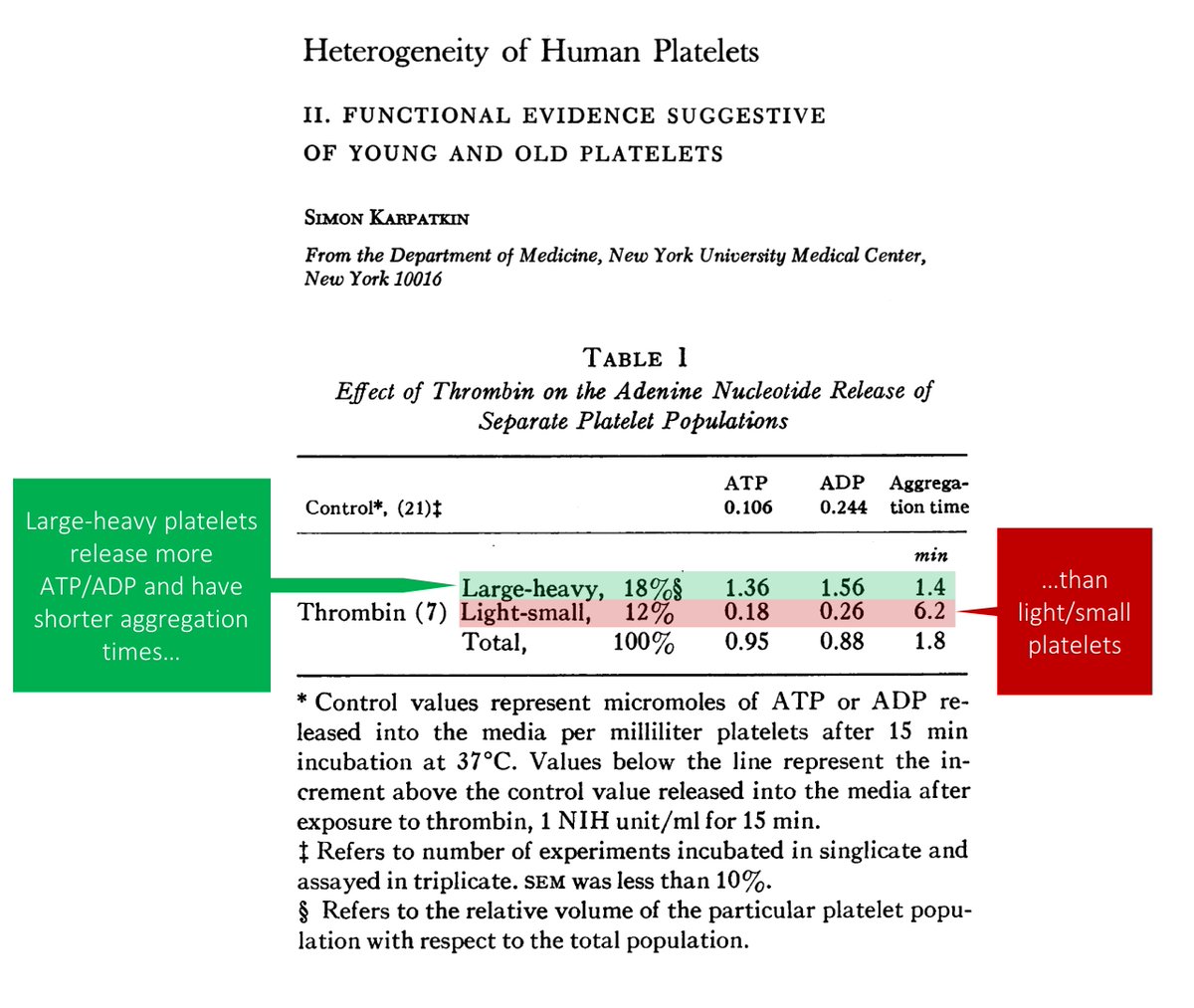
These large and heavy platelets release more ADP and ATP in response to thrombin, and have shorter aggregation times.
ncbi.nlm.nih.gov/pubmed/5771189
But, remember, ITP is a heterogeneous disease. While it's true that the risk of hemorrhage is low, some patients clearly bleed.
So: which lab finding might hint at an ITP patient with more of the younger platelets with superior function?
[IPF = immature platelet fraction]
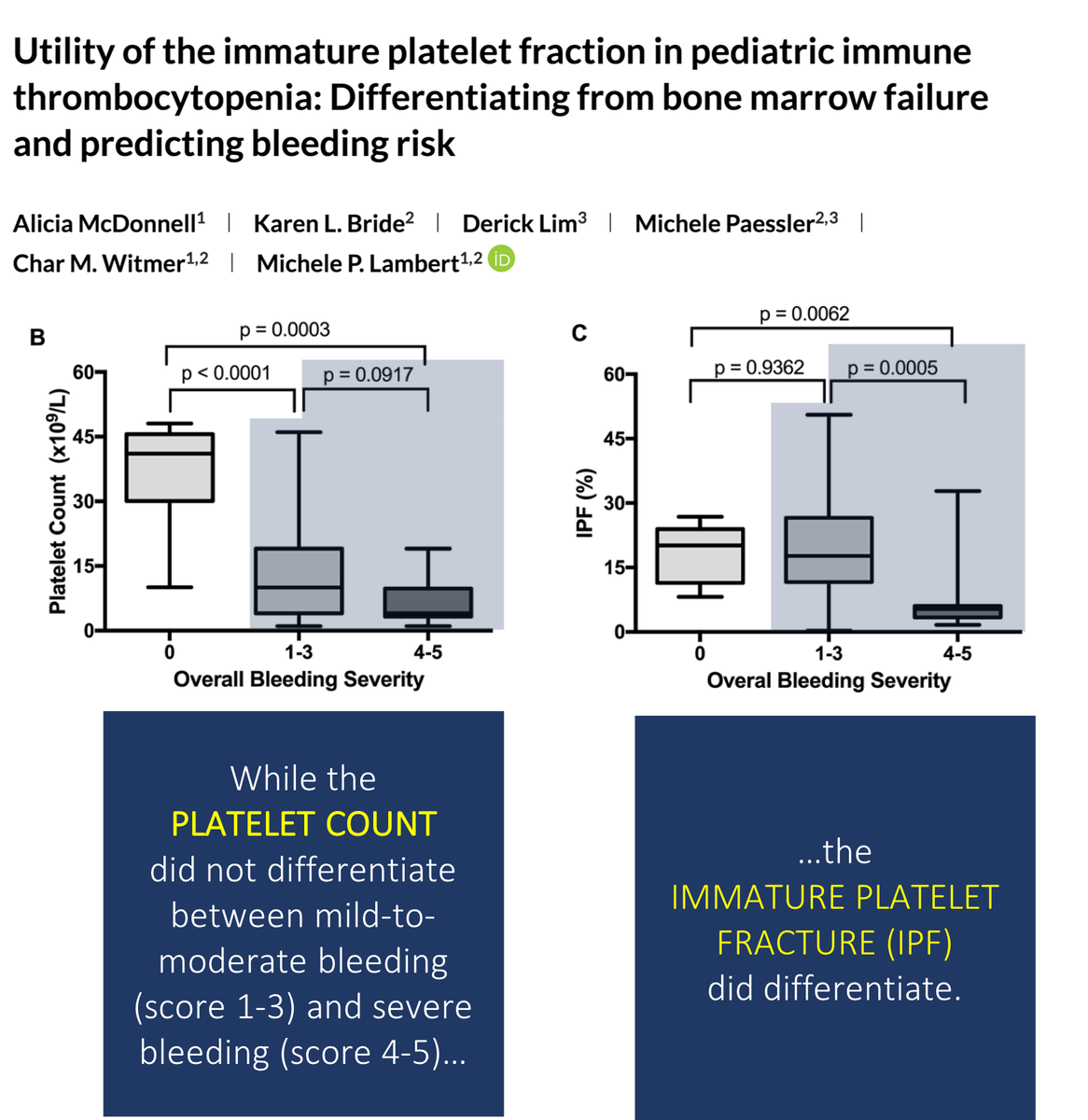
While not all studies agree, there is evidence that a high immature platelet fraction (IPF) is associated with less bleeding in ITP.
One pediatric study found that the IPF differentiates risk of severe bleeding better than the total platelet count.
ncbi.nlm.nih.gov/pubmed/28921855
I've never ordered an IPF.
But, there's another test that might provide a clue to a diagnosis of ITP. And this one has come with each of the thousands of CBCs I've ordered...
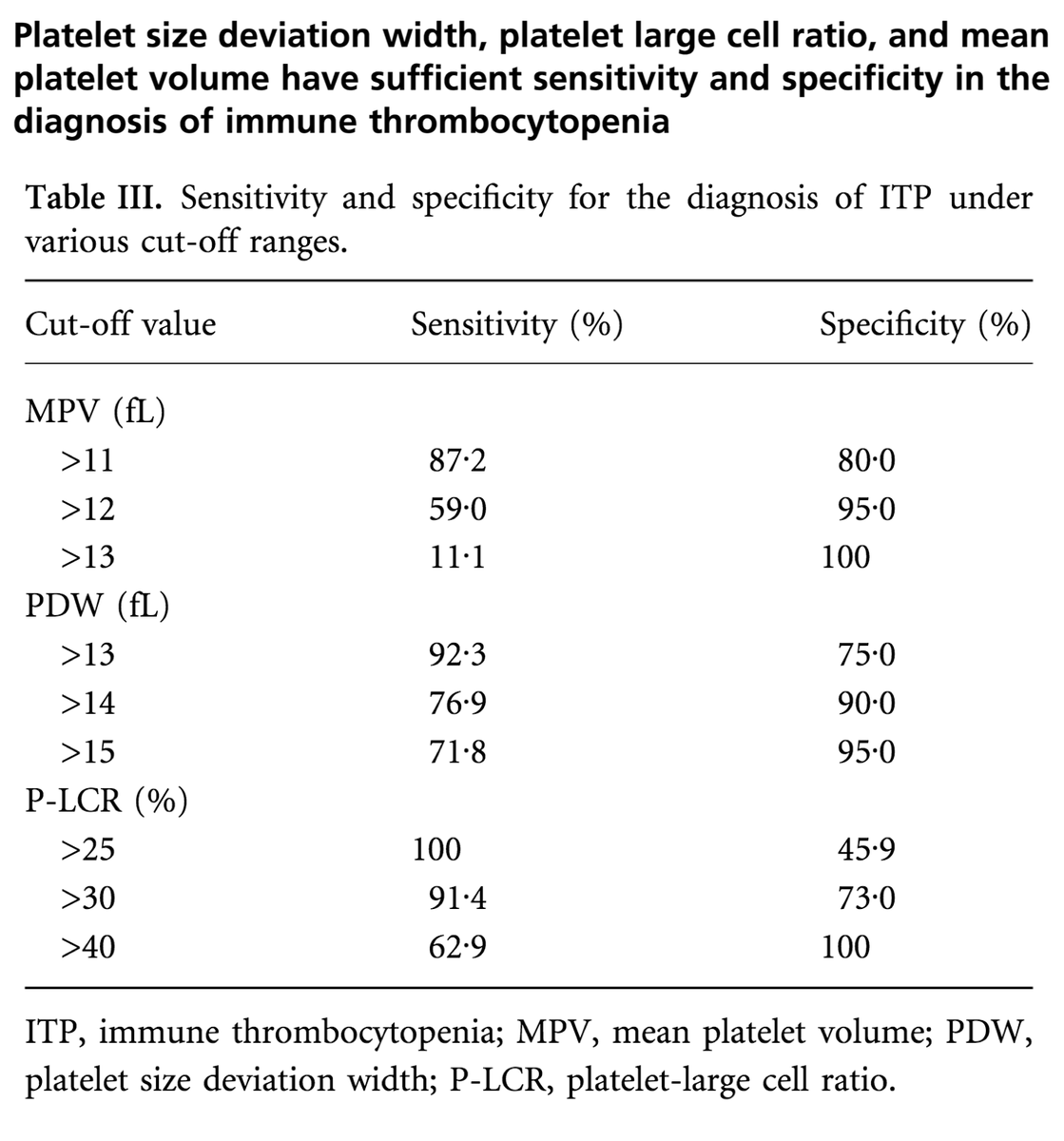
Mean platelet volume (MPV)! Higher MPVs suggest ITP.
ncbi.nlm.nih.gov/pubmed/15725092
One last thing: if ITP leads to more functional platelets, could these patients be at risk for thrombosis?
Maybe.
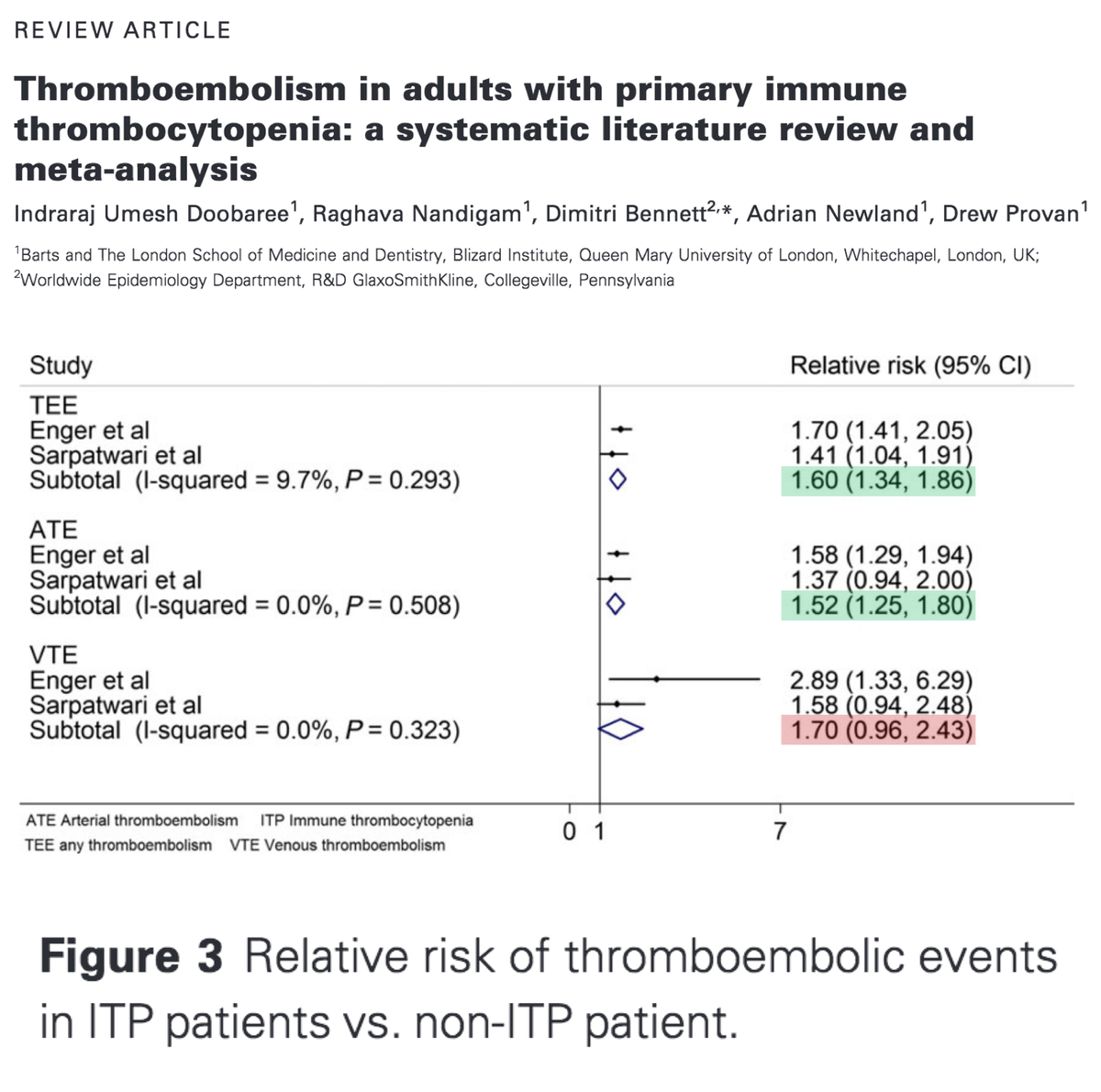
At least one meta-analysis demonstrated an increased RR for thrombosis. Whether this is due to ITP or associated factors isn't clear.
ncbi.nlm.nih.gov/pubmed/27199203
Before summarizing, here's the original question, posed one more time:
Which of the following is generally true of ITP, compared with bone marrow suppression?
Summary:
⭐️ITP is associated with young, big, immature, reticulated PLTs
⭐️These PLTs are, in general, more functional
⭐️This may lead to less severe bleeding at comparable PLT counts seen in bone marrow suppression
⭐️MPV and IPF may provide clues to diagnosis and risk