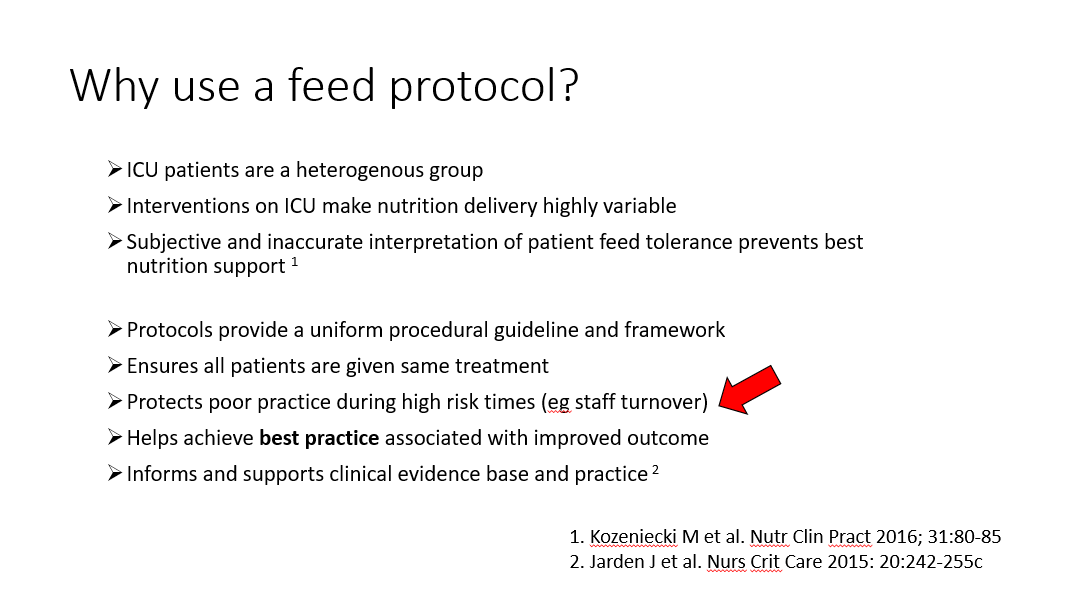
A useful summary of nutrition/malnutrition, immune function and critical care.
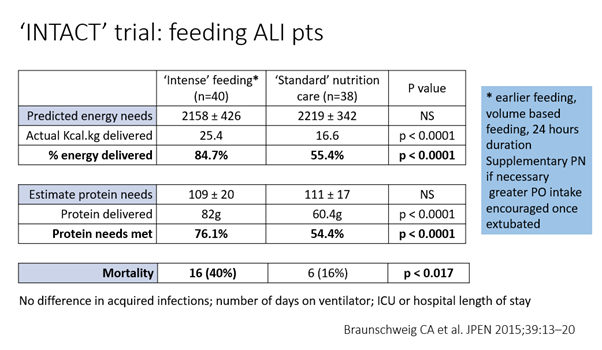
But in reality, #ICU is different... FWIW a personal interpretation of limited experience thus far..
Gastric emptying is related to osmotic load per unit time. Suggest start with 1kcal/ml feed. Then 'flip' to energy dense feed to match fluid restrictions once emptying established