1/ 🧵Wisdom in Medicine
What’s going on here? And why it’s key in #COVID19
It’s quite simple: we finally had the #wisdom to ask Mr. D the right question! He and his wife encouraged us to use this picture to teach what we learned.
#PalliativeCare #MedTwitter #NurseTwitter
What’s going on here? And why it’s key in #COVID19
It’s quite simple: we finally had the #wisdom to ask Mr. D the right question! He and his wife encouraged us to use this picture to teach what we learned.
#PalliativeCare #MedTwitter #NurseTwitter

2/ What we learned was to switch the preposition!
Mr. D was a pre-#COVID patient. On this day, he was taken off the vent after a MONTH. The incessant mantra had been, “What’s the matter WITH Mr. D?” He was surprised when we asked, “What matters TO you, Mr. D?”
Mr. D was a pre-#COVID patient. On this day, he was taken off the vent after a MONTH. The incessant mantra had been, “What’s the matter WITH Mr. D?” He was surprised when we asked, “What matters TO you, Mr. D?”
3/ He has a tracheostomy, as you can see. We insert this airway through the neck to improve #comfort when someone is on a vent well beyond 10 days. He’s more comfortable because he no longer has a tube in his mouth. We used a program called the #A2Fbundle to reduce his #delirium.
4/ The “trach” means he can’t run wind over his vocal cords to phonate (later we use a valve that allows him to speak). This doesn’t mean he can’t communicate. He’s a PERSON & I want to know him. Getting his #brain 🧠 to work is key to avoiding the ICU depersonalization chamber. 
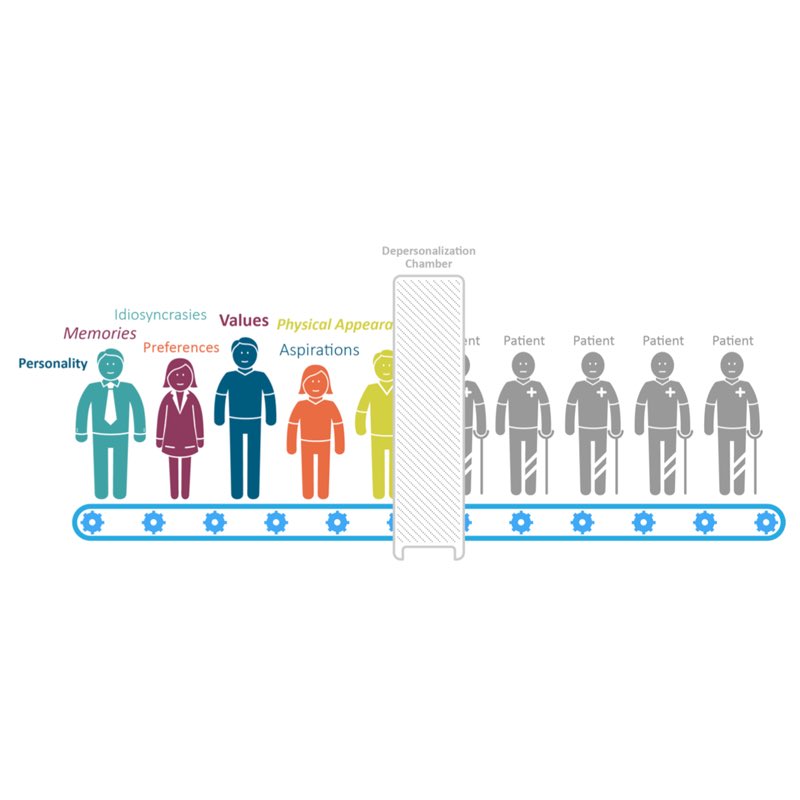
5/ Everything we do should be directed towards the whole person. #HUMANISM is key in the ICU, and for years I placed technology above humanism, which was flat-out wrong. I thought paternalistically, “I am right, and the patient doesn’t know as much as I do.” Pride. 😤 I am sorry.
6/ Back to this bit about #WISDOM. I’m not saying I’m wise. I’m not. But in this instance our team did find a bit of wisdom. How do I define wisdom?
7/ #Wisdom is being able to figure out how the consequences of my actions in the “now” will play out in the future for me or someone else. It involves me paying extra attention to the present rather than living in the past or the future. For Mr. D, it made a big difference.
7/ On this day, I asked, “What matters most to you?” He wrote down on a pad of paper, “My wife, Wanda, and I want a beer.” That’s what mattered TO him. Because we monitored him with a carefully designed test, we knew he was competent. It was key to respecting his personhood.
8/ You see his wife’s name is tattooed on his fingers, right?
W-A-N-D-A💥
So we got her to his bedside. Their hearts were sewn together, and this was right. Then I handed the #nurses a $10 bill and they said, “Now??” I retorted, “If not now, when?”
W-A-N-D-A💥
So we got her to his bedside. Their hearts were sewn together, and this was right. Then I handed the #nurses a $10 bill and they said, “Now??” I retorted, “If not now, when?”
9/ Not long afterwards, his amazing #nurse had him sipping this beer with Wanda at his side Precisely what he said mattered the most. They said thanks and “Doc, pay this moment forward to others.” So we took the pic...and I am...to you. 

11/ Why does this matter in the #COVID19 #Pandemic?
Because this lesson on exercising #Wisdom can apply to key decisions I face today: Do I get #Vaccinated or wear a #Mask? Why and why not? These are personal decisions. What matters most TO YOU?
👁 please read last tweet
Because this lesson on exercising #Wisdom can apply to key decisions I face today: Do I get #Vaccinated or wear a #Mask? Why and why not? These are personal decisions. What matters most TO YOU?
👁 please read last tweet
12/fin
Often, I have not exercised #Wisdom in doctoring my #COVID patients. Today I heard Mr. D whisper, “Dr. Wes, remember the beer! Pay it forward. Someone might benefit.” So here you go: What matters TO your patient? Ask the question & ACT on the answer.
#HOPE #COMPASSION
Often, I have not exercised #Wisdom in doctoring my #COVID patients. Today I heard Mr. D whisper, “Dr. Wes, remember the beer! Pay it forward. Someone might benefit.” So here you go: What matters TO your patient? Ask the question & ACT on the answer.
#HOPE #COMPASSION
• • •
Missing some Tweet in this thread? You can try to
force a refresh