Clinicians—have you ever responded to one of these?
Last week I left the hospital and boarded a flight for my vacation. I then responded to the mother of all in-flight emergencies…
Providing care in the air is a strange thing.
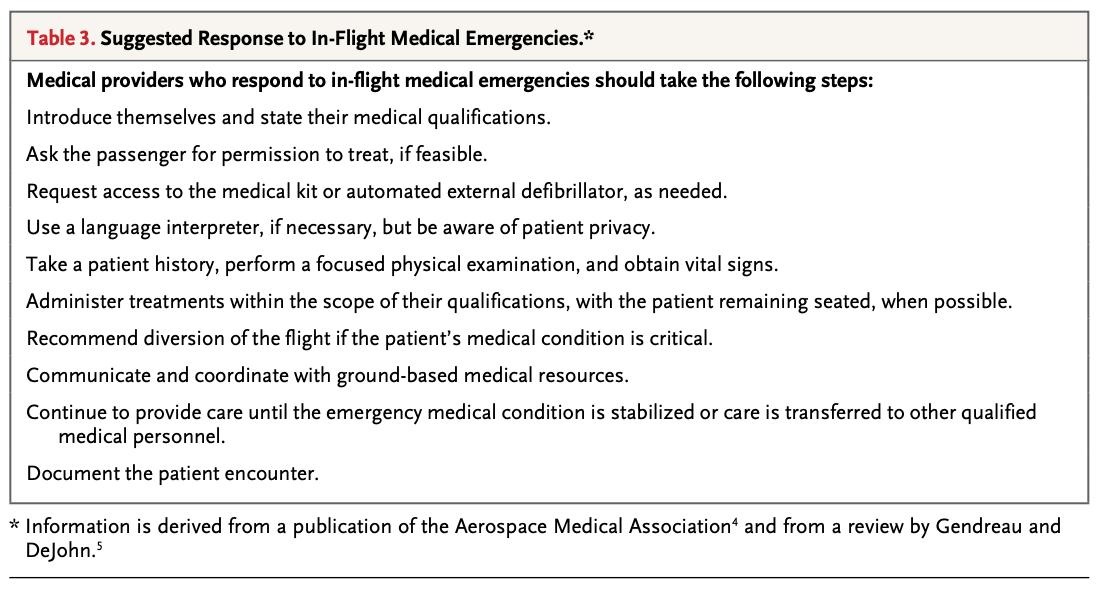
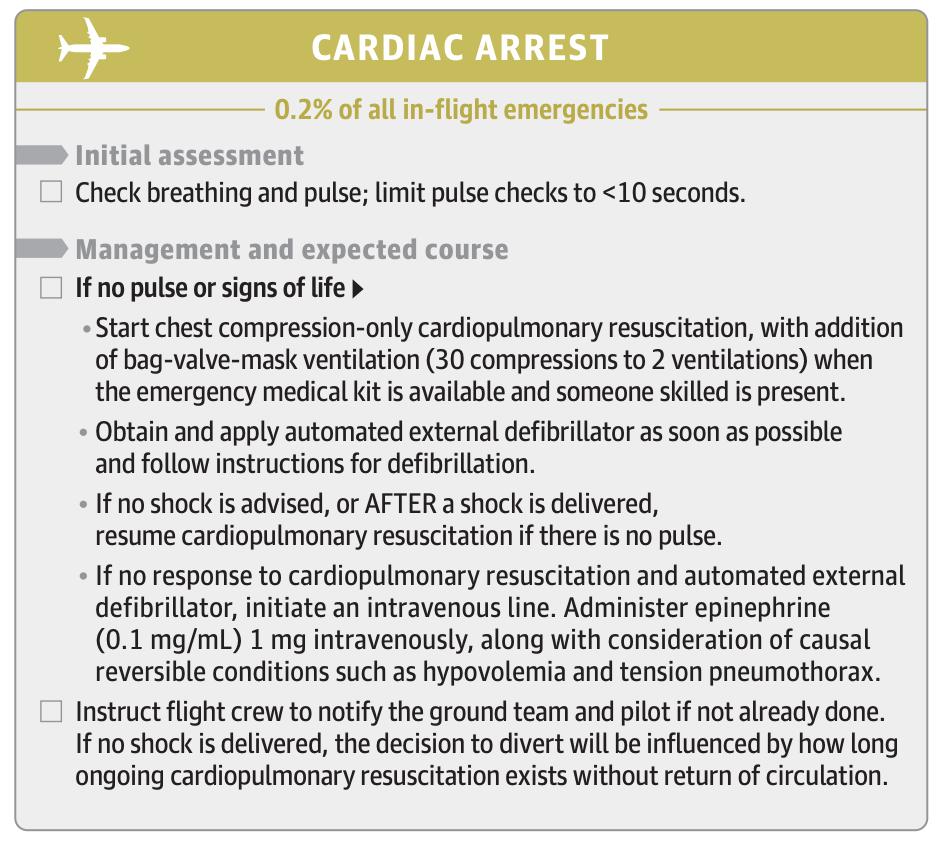
Martin-Gill. In-Flight Medical Emergencies: A Review: JAMA. 2018;320(24):2580-2590.
Peterson. Outcomes of Medical Emergencies on Commercial Airline Flights. NEJM 2013;368:2075-83.
Nable. In-Flight Medical Emergencies During Commercial Air Travel. NEJM 2015; 373:939-945
asma.org/asma/media/AsM…
#tweetorial #airtravel #inflightemergency #physician #womeninmedicine #MedTwitter
*Details of this event were changed to protect the privacy of all involved.