Bottom line is: the longer we wait to act, the more likely it becomes.
I've made some charts.
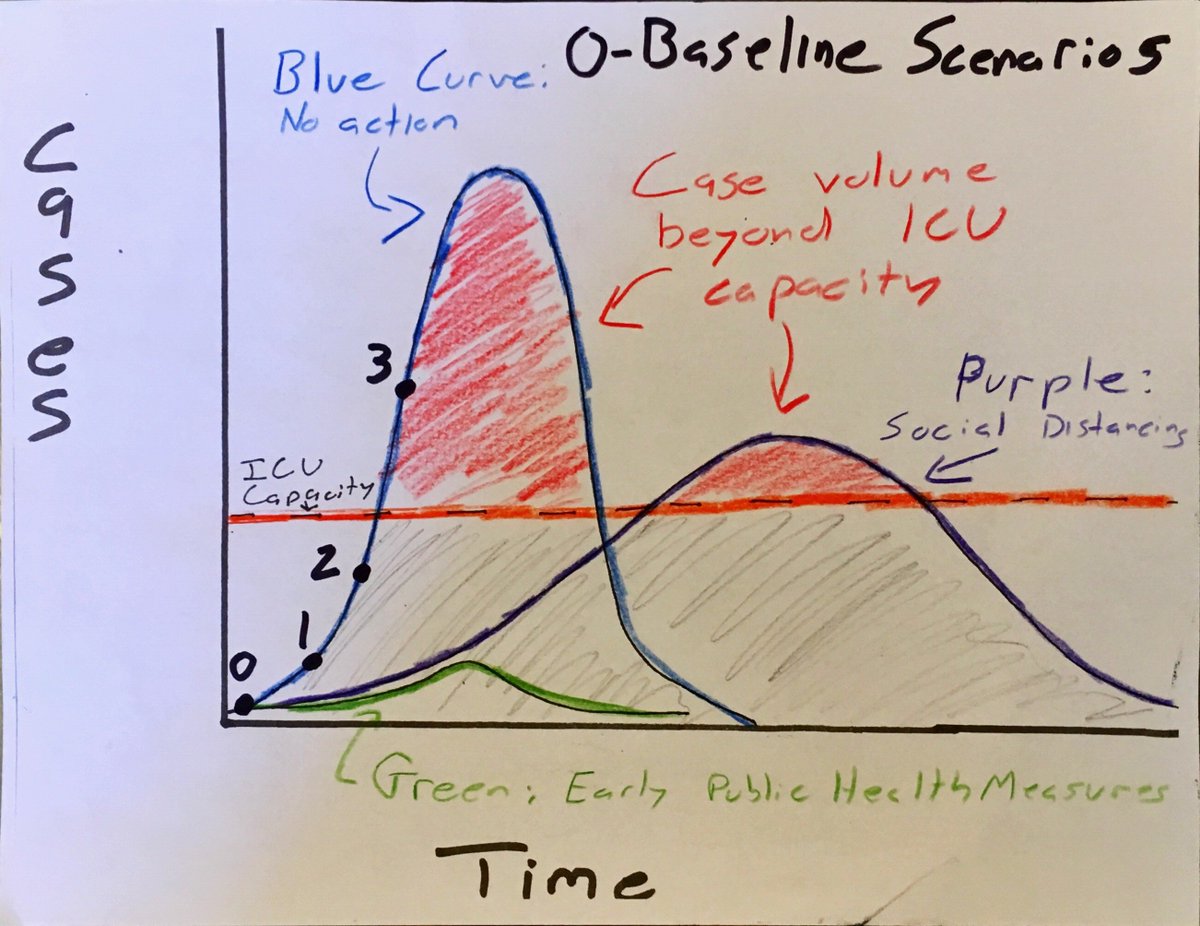
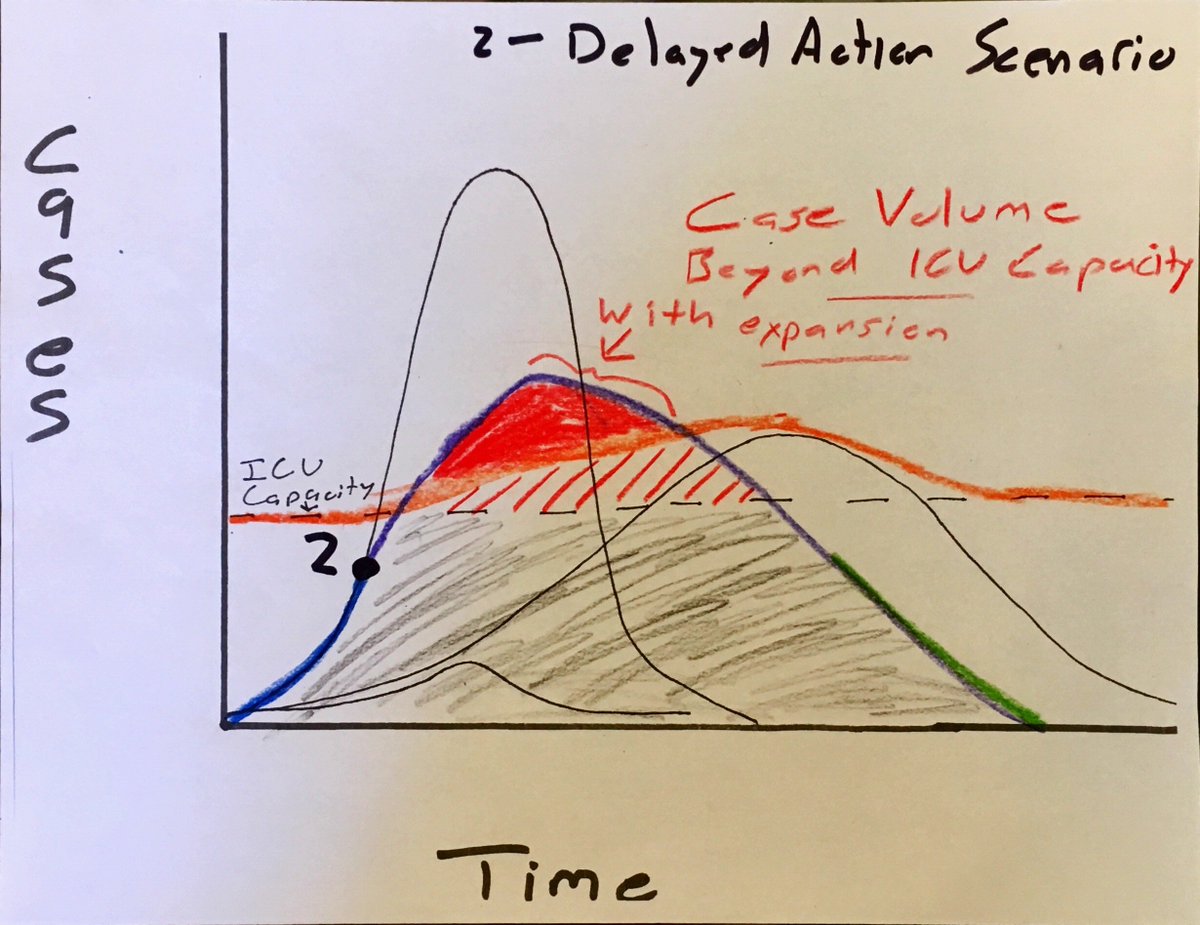
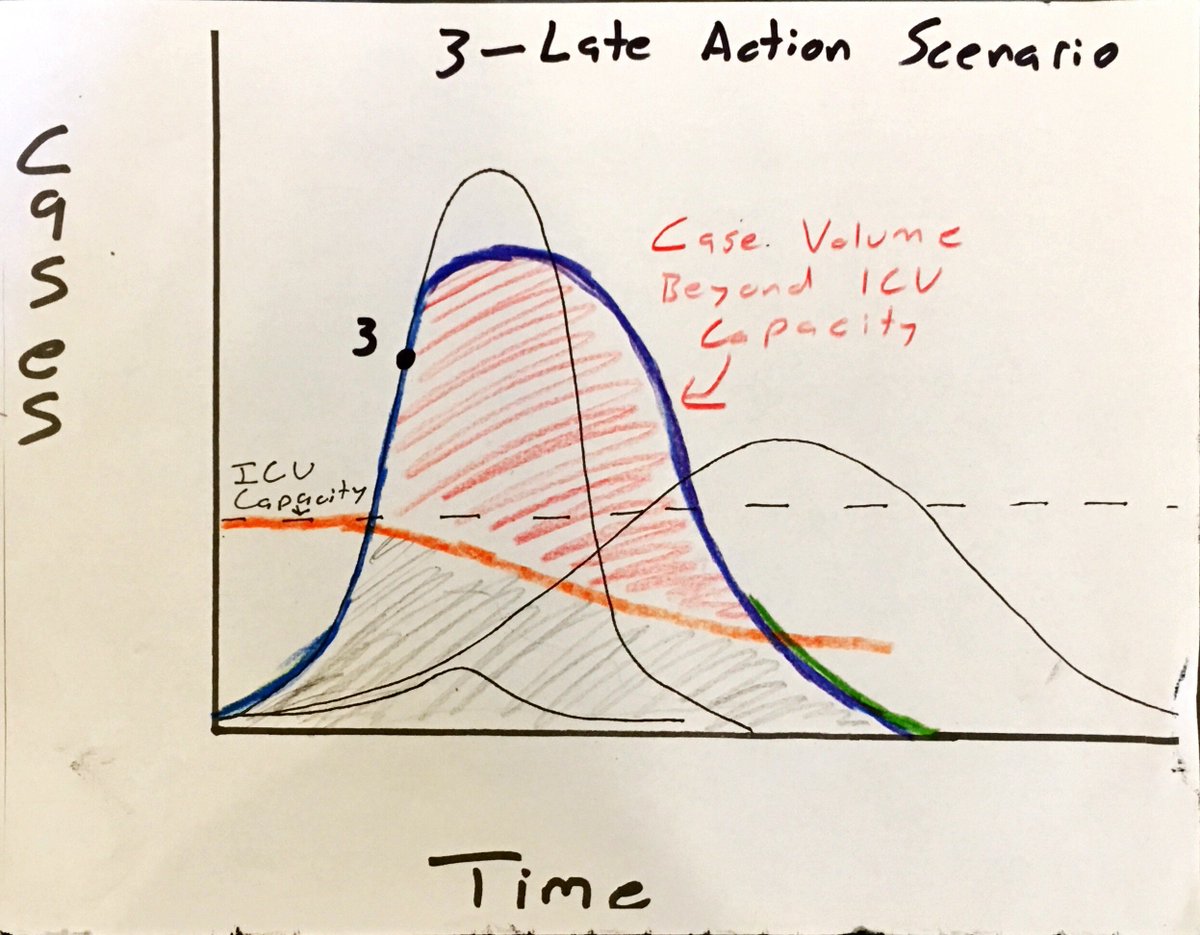
The red shading above ICU line represents new cases emerging beyond capacity. This is the greatest mortality risk.
And a 2015 paper estimates that ICU occupancy rates are on average around ~66%.
centerforhealthsecurity.org/cbn/2020/cbnre…
ncbi.nlm.nih.gov/pmc/articles/P…
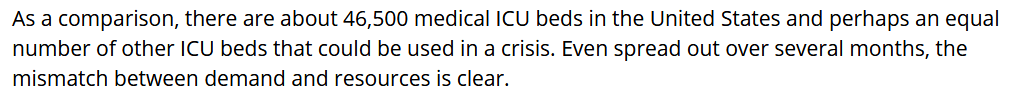
But for our purposes here, the takeaway is that ICU beds are limited and quite occupied already, but have some potential to stretch if given enough advance notice to expand capacity.
You trigger once virus' risk profile is understood, *and* this translates into political will for decisive action.
So these scenarios explore 3 points at which that may occur, and how timing of choice affects health outcomes.
Limits both case numbers and duration, and keeps cases below ICU capacity.
This minimizes overall mortality, and overall social disruption. Measures are still disruptive, but not as extreme as next scenarios.
And getting this back on track requires the most disruptive measures of any scenario.
We lost 6-7 weeks of potentially triggering earlier action, because lack of testing made us blind.
That's hugely important because extremity of actions must be calibrated accordingly.
So we're still losing time, even today.
/end